What is a plexus papilloma?

© Sergey Nivens - stock.adobe.com
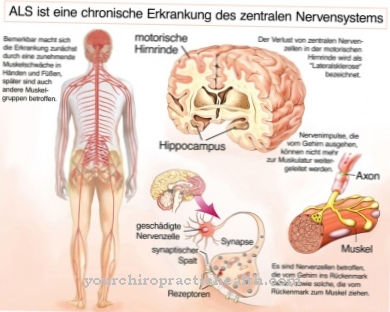
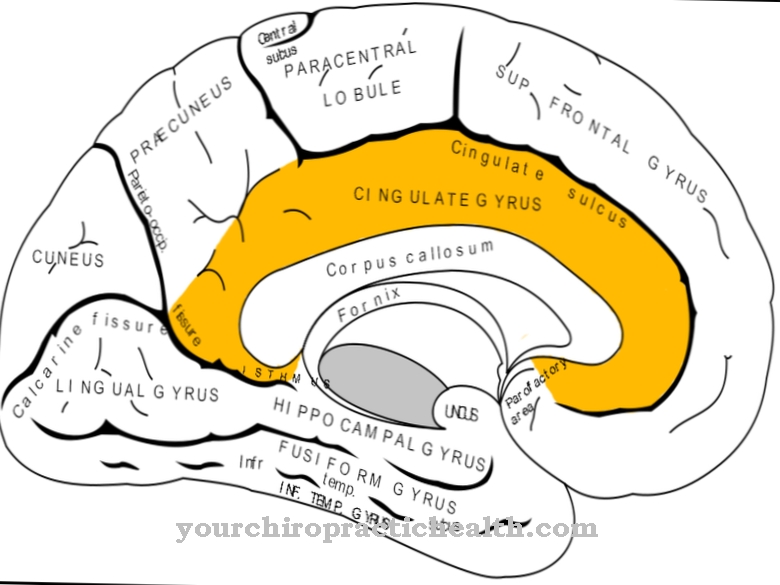
The rare benign (benign) plexus papilloma develops on the vein plexus that envelops the individual cerebral ventricles for supply and disposal. If left untreated, the nerve fluid (liquor) that circulates between the ventricles and is continuously exchanged is gradually impeded; above all, a disturbed drainage with a constant production rate of the liquor can lead to increased intracranial pressure with corresponding symptoms.
In addition, the space required by the plexus papilloma puts pressure on certain areas of the brain and leads to symptoms including functional failure. Infants under 2 years of age and children up to the age of around 12 are particularly affected, with girls and boys equally affected. The plexus papilloma can be surgically removed with a good subsequent prognosis. The benign plexus papilloma contrasts with the malignant plexus tumor, which tends to recur even after surgical removal.
causes
The relative rarity of plexus papilloma or plexus carcinoma has so far not shown any statistical abnormalities with regard to possible triggering factors for their development. Tumor research has not made good progress in this area because there are obviously no clear starting points. From time to time attempts are made to blame certain gene mutations.
For example, attempts have been made with little success to link plexus papillomas to Aicardi syndrome or Li-Fraumeni syndrome. The Aicardi syndrome is an X-linked hereditary disease that leads to undesirable developments in the brain and the autosomal dominant, i.e. not gender-typical, inherited Li-Fraumeni syndrome leads to a high probability that those affected will develop multiple tumors at a young age get sick.
Another research approach has been to try to attribute the development of a plexus papilloma or carcinoma to certain viral infections. This approach did not yield any reliable findings either. As a conclusion, it can be stated that there is (yet) no scientifically proven knowledge about the causes of a plexus papilloma or carcinoma.
Symptoms, ailments & signs
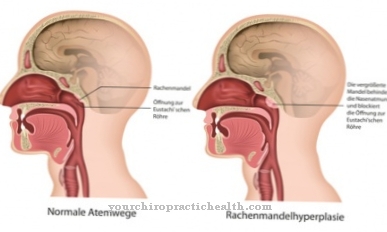
The location of a plexus papilloma on one or more cerebral ventricles means that symptoms that are initially unspecific, but nonetheless typical, occur at an early stage of the tumor. It is above all the papilloma itself that, due to its volume, hinders the circulation or the outflow of the liquor. At the same time, the papilloma tissue also produces additional brain water, so that the inflow and outflow of the liquor are no longer in harmony with each other.
Initially there is an increase in intracranial pressure, which leads to the unspecific symptoms of headache, nausea and vomiting, seizures and irritability. Especially in small children, for whom it is difficult to classify the unspecific symptoms correctly, untreated in an advanced stage can lead to the formation of a hydrocephalus.
The direct pressure that the plexus papilloma exerts on the surrounding brain area can also lead to neuronal functional disorders that cause disorders or failures of certain motor and / or sensory abilities.
Diagnosis & course of disease
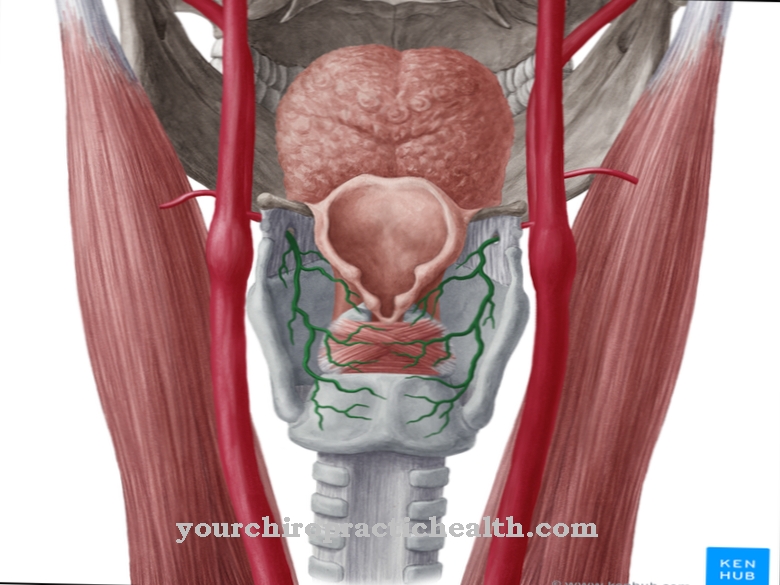
If the unspecific symptoms described above occur, which cannot be assigned to a specific disease, there is a suspicion of a neurological disease in the brain. While an electroencophalogram (EEG) shows the first signs of whether and where a brain tumor might be present, the imaging methods computed tomography (CT) and magnetic resonance imaging (MRI) allow more precise statements.
The focus of diagnostics is shifting from CT to MRT because the soft structures are more clearly depicted by the MRT. An MRI can give a good picture of a plexus papilloma. The tissue of the tumor stands out as a homogeneous mass with a cauliflower-like structure. An analysis of the cerebrospinal fluid can provide information about whether there is an inflammation of the nerves that led to the symptoms.
A biopsy with a subsequent subtle examination can provide final certainty as to whether the tumor is benign or malignant. Ultimately, the only effective treatment option is the complete surgical removal of the tumor.
Complications
In the plexus papilloma, complications usually only arise if the disease is left untreated. In this case, self-healing does not occur, so that surgical removal of the tumor is necessary. If the tumor is not removed, high pressure in the brain can result and the various brain areas fail. This means that those affected usually suffer from paralysis and other motor disorders.
The high pressure in the brain also leads to severe headaches and not infrequently to vomiting and nausea. Those affected themselves also suffer from cramps and significantly increased irritability. A head of water can also form through the plexus papilloma if the water is not removed from the brain. Without treatment, the brain is irreversibly damaged by the plexus papilloma.
Treatment is usually not associated with any particular complications. The tumor can be removed by surgery. Usually there are no other complaints. Those affected may have to rely on radiation therapy after treatment. Successful treatment does not affect the patient's life expectancy.
When should you go to the doctor?
Since a plexus papilloma is a tumor, it must always be examined and treated by a doctor. This disease does not heal itself and the person concerned usually dies if there is more water retention in the brain. An early diagnosis and treatment of the plexus papilloma has a very positive effect on the further course of this disease and can prevent complications.
The doctor should be consulted in the case of plexus papilloma if a lump develops on the head of the person concerned. The patients suffer from headaches and nausea, although these symptoms occur for no particular reason and do not go away on their own. Here, pain killers cannot relieve the pain either. A head of water also indicates the plexus papilloma and should always be examined by a doctor. In the further course there are also motor failures, which also indicate the brain tumor.
The examination and diagnosis is usually done with the help of an MRI. However, further treatment is carried out in a hospital by means of an operation. Whether the plexus papilloma will reduce the patient's life expectancy cannot generally be predicted.
Therapy & Treatment
Since there is no way to kill a plexus papilloma by drugs or other means, if the diagnosis is clear, the only effective treatment option is complete surgical removal of the papilloma. Only in a few cases can an artificial drainage of the CSF, which reduces the intracranial pressure, achieve a significant alleviation of the symptoms.
Specialized centers are able to remove the tumor as gently as possible by microsurgical means or endoscopically. The aim is to enable the circulation of the brain water again by reopening possible drains. During the operation, so-called neuronavigation and imaging methods are used to increase safety and tissue protection, which enable constant monitoring of the surgical procedure.
There is no consensus among experts as to whether a postoperative continuation of the treatment with radiation therapy is necessary and useful.
prevention
Because no clear trigger factors for the development of a plexus papilloma are known and also viral diseases or genetic predispositions could not be proven as causers, there are no preventive measures that could prevent the tumor from developing.
However, as toddlers and children under 12 are mostly affected, persistent and recurring symptoms such as headaches, malaise and possible personality changes that cannot be assigned to other diseases should also be well clarified neurologically.
Aftercare
In most cases, those affected have only a few or limited direct follow-up measures available for a plexus papilloma. Therefore, the person affected should consult a doctor at the first symptoms or signs of the disease in order to prevent further symptoms or complications from occurring. It cannot heal on its own, so treatment by a doctor is always necessary.
In most cases, those affected are dependent on an operation. The child should then take it easy and rest. Exertion or stressful physical activities should be avoided in order not to unnecessarily burden the body. Even after a successful procedure, regular checks and examinations by a doctor are necessary in order to identify and remove further tumors at an early stage.
The children have to be supported especially by their parents and relatives during therapy. This can also prevent possible psychological upsets or depression. If the plexus papilloma is recognized early and treated correctly, the affected person usually does not experience a reduced life expectancy.
You can do that yourself
The plexus papilloma occurs in children and young children. Naturally, they are not sufficiently capable of taking self-help measures that would result in healing. Therefore, legal guardians, relatives or people close to them from the social environment are increasingly responsible for improving the situation in the interests of the child by taking various approaches.
An open approach to the disease is indicated in everyday life. Risk factors and the overall circumstances should be sufficiently and clearly explained to the child. Open questions must be answered honestly and informatively. This behavior prevents irritations or unpleasant surprises. With a sufficient flow of information, dealing with the disease is often better.
Since a hospital stay is necessary for the treatment of the brain tumor, measures should be taken to promote well-being and zest for life. Games and fun are to be integrated daily as far as possible. A positive attitude among adults has a positive effect on the child. It has a motivating effect and reduces discomfort and fears. Contact with peers and other sick people can be perceived as pleasant by the child.The mutual exchange of experiences created creates opportunities for better coping with the overall situation.

.jpg)







.jpg)