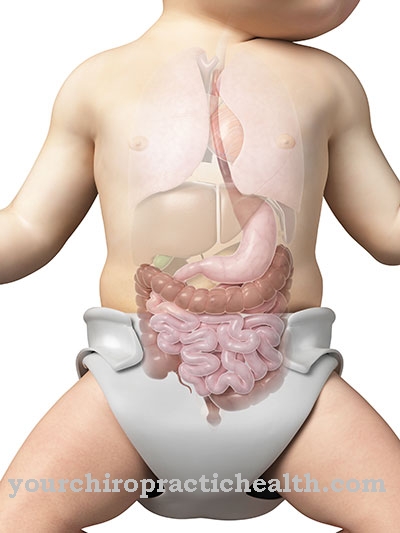
The Narrowing of the stomach door or. Pyloric stenosis is a thickening of the passage from the stomach to the duodenum. It prevents the food from passing through and leads to gushing vomiting. Pyloric stenosis must be treated, otherwise it can cause a life-threatening condition.
What is pyloric stenosis?
.jpg)
© nicolasprimola - stock.adobe.com
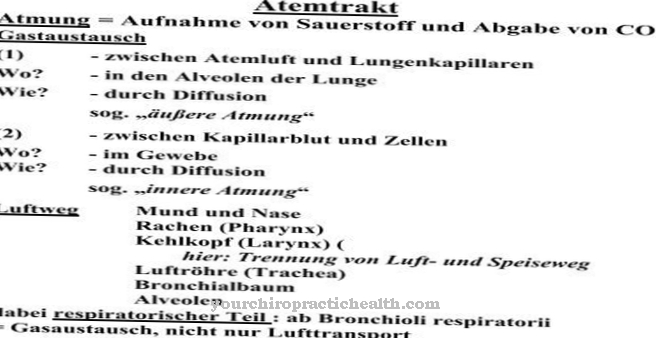
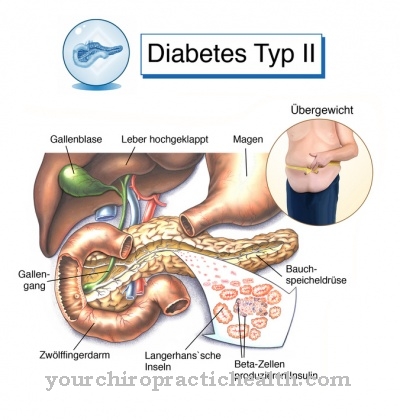
The Narrowing of the stomach door (medical: Pyloric stenosis) is a thickening at the exit of the stomach. The gastric gate (pylorus) is a muscle that can be closed and opened like a ring by contracting and relaxing thanks to circular fibers.
The pylorus separates the stomach from the duodenum. If the stomach gate is thickened, it can no longer be opened far enough to allow the chyme to pass into the intestines. This leads to the fact that the digested food remains in the stomach, begins to ferment there and putrefactive processes begin.
The narrowing of the stomach door is common in infants from the second to eighth week of life, with boys being more often affected than girls. Adults can also suffer from narrowing of the pelvic door, usually this is caused by scarring after the gastric or intestinal ulcer has healed.
causes
The exact cause of the Narrowing of the stomach door is not known. The disease is believed to be genetic in infants because it has a family history.
This means that in a family in which one of the parents already had a narrowing of the stomach door, the offspring are often also affected. If the gastric gate narrowing occurs in adults, the cause is often scarring of the pylorus. These sometimes arise after ulcers in the stomach or duodenum.
If they are near the gastric porter, scars may form on the pylorus as it heals. They thicken the sphincter muscle and the narrowing of the gastric gate arises. Another possible cause of a narrowing of the stomach door is the development of tissue directly at the stomach outlet.
Symptoms, ailments & signs
A typical symptom of pyloric stenosis is gushing vomiting shortly after eating a meal. This can lead to repeated vomiting, which takes place at short intervals. Usually the odor of the stomach contents is very sour. If the stomach is already irritated, there may be isolated traces of blood in the vomit.
Since the stomach outlet is often thickened in pyloric stenosis, it can be clearly felt through the abdominal wall. You can also occasionally see the stomach muscles contract, which can be observed as a wave-like movement of the abdomen. Since the vomit is excreted in addition to food, the children quickly suffer from deficiency symptoms.
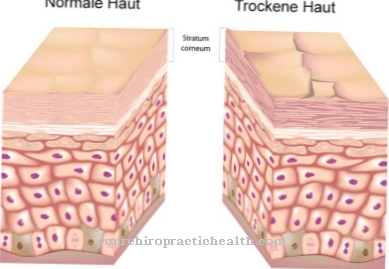
You lose weight and are very thirsty, which manifests itself in downright greedy drinking. However, since they do not retain the fluid, the typical signs of dehydration such as dark circles, dry mucous membranes and so-called standing skin folds appear over time.
The latter are folds of the skin drawn with fingers that remain when you let go. There is also severe pain in the upper abdomen. Sometimes jaundice can also occur, which is accompanied by yellowing of the skin and the originally white dermis of the eyes. All symptoms lead to total exhaustion over time and require urgent medical treatment.
Diagnosis & course
_2.jpg)
The typical symptom of Narrowing of the stomach door in infants, gush-like vomiting occurs approximately 30 minutes after eating. The smell of the vomit is very sour and sometimes thin blood threads are visible.
Occasionally one can see the undulating movements of the stomach through the abdominal wall as it tries to empty itself through muscle contractions. The children feel unwell and have abdominal pain. As the vomiting disrupts the intake of food and fluids, the child loses weight and shows signs of dehydration (desiccosis) such as dry mucous membranes, a sunken fontanel (soft spot on the top of the head) and dark circles.
Adults with a narrowing of the gatekeeper feel thirsty and suffer from a feeling of fullness, they have to burp sour and, like children, vomiting occurs in a torrent. The doctor makes the diagnosis based on the symptoms and the medical history. With the help of an ultrasound examination, he can determine whether there is a narrowing of the stomach door, as the thickened sphincter muscle is visible on the ultrasound.
A blood test is used to clarify whether the lack of fluid has already resulted in a lack of vital electrolytes and minerals.
Complications
In the worst case, the pyloric stenosis can lead to death. However, this case usually only occurs if treatment is not initiated. Patients experience persistent vomiting due to the thickening. It is not uncommon for depression or irritability of the person concerned to occur.
Pain in the abdomen and the epigastric region can also occur and significantly reduce the patient's quality of life. Vomiting occurs mainly after ingesting food. Persistent vomiting inevitably leads to severe weight loss for those affected.Young children often cry because of the pain, so that the parents and relatives of the child are usually stressed and irritated as well.
Pyloric stenosis can also lead to increased thirst and a feeling of fullness. Weight loss also leads to various deficiency symptoms, which have a very negative effect on the patient's health. The disease is usually treated with surgery without complications. The symptoms disappear completely and do not reappear. The life expectancy of the patient is not restricted either.
Treatment & Therapy
The Narrowing of the stomach door is usually treated surgically. Conservative therapy, i.e. non-operative treatment, can only be used for very slight constrictions. It consists of feeding the patient only very small portions of food and administering medication to relax the muscles.
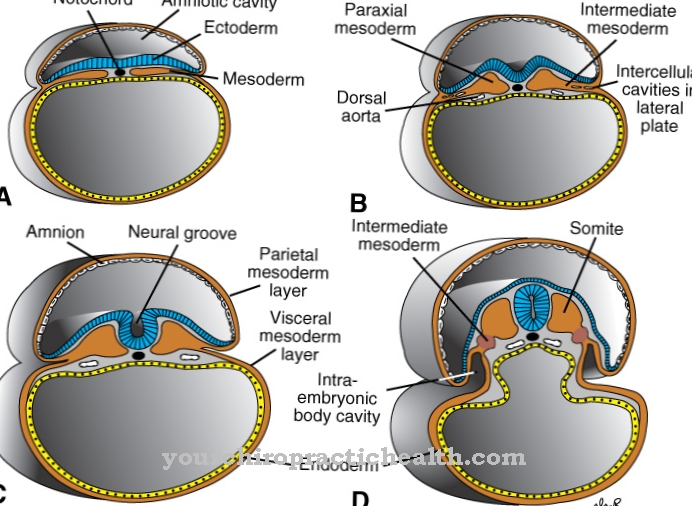
This therapy is very tedious and usually does not bring the desired success. In most cases, an operation is performed, but this is only possible after the patient has been stabilized by the administration of electrolytes and liquid food. In a surgical procedure called pyloromyotomy (myo = muscle, tomie = cut), the ring-shaped muscle of the gastric porter is divided and pulled open with one cut.
This increases the diameter of the passage. The operation can be performed with an incision in the abdomen (laparotomy) or with a laparoscopy (laparoscopy). During the laparotomy, the abdominal wall is opened in order to get to the gastric porter. During laparoscopy, only three small incisions are made in the abdomen, through which a camera and the surgical instruments are introduced to the gastric porter. After surgery to narrow the stomach door, you can start eating solid food again after a few days.
You can find your medication here
➔ Medicines against vomiting and nauseaprevention
One Narrowing of the stomach door cannot be prevented as it is either congenital or caused by scarring. It is important to consult a doctor immediately if you suspect a narrowing of the doorway, as the disease can lead to a life-threatening condition if left untreated.
Aftercare
Follow-up treatments and any follow-up examinations depend on the treatment method used. In most cases, this affects infants who are treated surgically, for example in a laparoscopic procedure. As a rule, infants recover from the procedure very quickly, so that a gradual increase in nutrition can take place postoperatively.
The symptoms observed before the operation disappear quickly and the risk of a recurrence, i.e. a recurrence of the pyloric stenosis, is not to be feared. Pronounced follow-up recommendations are therefore not given. If the typical symptoms recur, they should be used as an opportunity to have more detailed examinations carried out. In less severe cases where no surgical treatment is indicated, the symptoms that suggest pyloric stenosis should be carefully monitored.
In the very rare cases in which surgical treatment is urgently indicated but is not possible due to other diseases, the only option is a jejunal feeding tube. It flows directly into the small intestine, bypassing the gastric gate (pylorus). In these cases, follow-up care is expanded to include ongoing care as long as the treatment of the secondary disease that prevents the primary surgical procedure continues.



.jpg)
.jpg)







.jpg)