The Tarsal tunnel syndrome - also called nerve compression syndrome or bottleneck syndrome - denotes damage to the tibial nerve. It runs through the foot and causes painful discomfort due to damage or irritation.
What is tarsal tunnel syndrome?

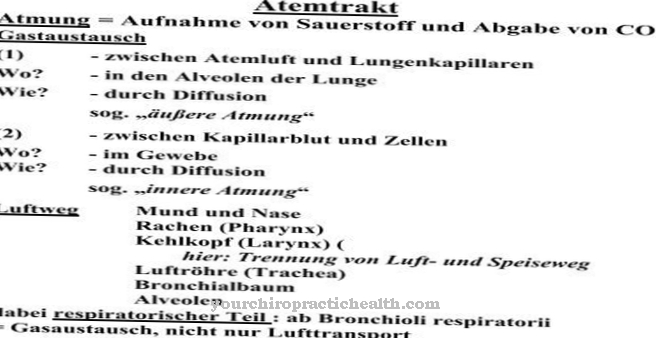
© SciePro - stock.adobe.com The medic calls under Tarsal tunnel syndrome damage to the tibial nerve (Tibial nerve). The localization is predominantly in the ankle. In this area, the tibial nerve runs through the tarsal tunnel. The tunnel is formed by a tight ligament that runs through the inner ankle of the foot. The tibial nerve is responsible for controlling the muscles of the sole of the foot, whereby the muscles of the lower leg (which are used to bend the leg, for example) are also dependent on the tibial nerve.
As a result, all perceptions that are present in the lower leg area are passed on via the central nervous system. If permanent pressure is exerted on the nerve in the tarsal tunnel, the tarsal tunnel syndrome develops. The lower leg as well as the foot are mainly affected.
causes
In around 80 percent of all cases, a cause is found that is responsible for the tarsal tunnel syndrome. Above all, it is benign bone outgrowths (which subsequently narrow the so-called tarsal tunnel) or injuries. In a few cases tumors are responsible; Inflammation in the region of the tarsal tunnel can also trigger the syndrome.
The tarsal tunnel syndrome is favored by foot-stressing sports, a flat arched foot or injuries to the ankle and osteoarthritis. Diabetes mellitus or varicose veins are among the favorable factors. Tight, too high or rigid shoes, such as skiing, mountain or hiking boots, can also be a trigger or significantly worsen the syndrome.
Symptoms, ailments & signs
The tarsal tunnel syndrome is mainly noticeable through abnormal sensations that occur during the night. Those affected complain of a feeling of numbness, constant tingling or even a burning sensation, whereby the region of the foot is mainly indicated. Sometimes those symptoms can also radiate (calves); the area of the inner ankle is permanently sensitive to pain. The symptoms can be exacerbated by standing or walking for long periods of time. However, if the foot is elevated, the pain disappears.
The symptoms appear at irregular intervals at the beginning. Only in the further course of the disease do the persistent phases increase; the nerve continues to be damaged, making the pain permanent. As a result, the affected person feels a significant muscle weakness, so that the foot movement can no longer be performed correctly.
Diagnosis & course of disease
If a tarsal tunnel syndrome is suspected, a doctor must be consulted immediately. Only with timely treatment is it possible that further nerve damage can be prevented. The attending physician, ideally an orthopedic surgeon, will ask the patient various questions that make up part of the anamnesis. For example, since when the person concerned has been suffering from the symptoms and when they take on a particular intensity.
The doctor then examines the foot. Only by “knocking” the inner ankle is it possible for the person affected to report pain. If the muscles are weak, this can be the first sign of local inflammation. Swelling and warmth are also indications that it could be a tarsal tunnel syndrome.
The doctor checks the muscles using ENG - electroneurography. That exam will check the speed and impulse of the nerve. The diagnosis of tarsal tunnel syndrome can be confirmed by an X-ray. In many cases, an MRI - magnetic resonance imaging - can provide information about whether it is the so-called syndrome.
If the tarsal tunnel syndrome is treated too late or not at all, the symptoms worsen. The nerve suffers irreversible damage. For this reason it is important that treatment takes place as early as possible. If permanent damage has already occurred, which mainly affects the shin nerve, even an operation can no longer relieve the symptoms.
Complications
First and foremost, those affected by the tarsal tunnel syndrome suffer from various paresthesia and sensory disorders. These have a very negative effect on the quality of life and can lead to restrictions in movement and in everyday life in general. A feeling of numbness can also set in and those affected often suffer from a tingling sensation or a burning sensation in the respective region.
The pain can also radiate into the calves. Often the symptoms do not only occur when walking, but also when standing or sitting. At night, the symptoms of the tarsal tunnel syndrome can lead to insomnia and thus irritability in the person concerned. If left untreated, the tarsal tunnel syndrome leads to muscle weakness, whereby normal movements of the foot can no longer be carried out easily.
If the nerve is irreversibly damaged, no further treatment is usually possible. The treatment itself takes place with the help of cortisone and can limit the symptoms. In the case of a tumor, it must be surgically removed. As a rule, patients are dependent on therapies even after successful treatment.
When should you go to the doctor?
If there are irregularities in the shin or lower leg, the processes should be monitored further. If there is a one-off overload of the organism, the symptoms will be alleviated after a period of rest or rest. If, after a restful night's sleep, permanent symptom relief is achieved, there is in most cases no need for a medical check-up. In the future, physical activities should be oriented towards the needs of the organism.
If symptoms or irregularities persist over a long period of time or if they increase in scope and intensity, a doctor should be consulted. A tingling sensation on the skin or a burning sensation indicate a health condition that needs further investigation and treatment. Pain, hypersensitivity to touch stimuli or a decrease in physical performance should be examined and treated. If the person concerned complains about irregularities of the inner ankle and the foot, this is considered to be a sign of an existing disease.
Disorders of general movement sequences and a general feeling of illness should be discussed with a doctor. If pain increases while moving, the cause must be clarified. If, due to the impairments, the daily obligations or usual sporting activities can no longer be performed, a medical examination should be initiated.
Therapy & Treatment
The doctor must ensure that he reduces the so-called mechanical pressure that is on the nerve. With shoe insoles it is possible that the load that the foot has to carry is “passed on” to the outside so that the inner foot perceives a relief. Medicines are used to combat and alleviate the symptoms, but do not treat the cause.
Inflammatory processes are mainly treated with cortisone; the surrounding tissue, which is swollen, may become swollen with the administration of cortisone. The nerve can be relieved by the swelling. Conservative treatment is used for around two months. If there is no significant improvement in the situation afterwards, the doctor must inform the person concerned that the tarsal tunnel syndrome can also be treated surgically.
As part of the operation, the tight ligament surrounding the tarsal tunnel is removed. In a few cases, parts of the nerve covering also have to be split. Tumors or excess bones must also be surgically removed. After the operation, it is important that the patient relieves the pressure on the foot using crutches.
The success of the operation also depends on the concomitant diseases that have led to the tarsal tunnel syndrome. The rehabilitation lasts six months; in some cases another operation is necessary.
You can find your medication here
➔ Medicines for painprevention
The tarsal tunnel syndrome cannot be prevented if it is caused by injuries or tumors or bone outgrowths. Good footwear is important (no long-term wearing of high or stiff shoes) and the treatment of diseases that can promote tarsal tunnel syndrome.
Aftercare
If the tendinosis calcarea has to be treated surgically, follow-up care is extremely important. After the surgery, the affected shoulder should be spared for about three weeks. To treat the pain, the patient is given drugs that have analgesic and anti-inflammatory effects.
The following physiotherapeutic exercises are an important part of the aftercare of a calcified shoulder. They take place after the acute pain has subsided. After the tendon has healed, a pain-adapted mobilization treatment is carried out. If passive exercises are carried out in the first phase of therapy, active exercises are carried out in the second phase, which are useful for achieving full freedom of movement of the shoulder joint.
Pain-adapted therapy is understood to mean exercises that only load the shoulder as much as the pain allows. The pain threshold must not be exceeded. The postoperative follow-up treatment also includes a third phase. Within this framework, the stability, strength and muscle coordination of the affected shoulder can be completely restored.
After a calcified shoulder surgery, the pain usually subsides after 24 to 48 hours. Therefore, further follow-up treatment, which is carried out on an outpatient basis, can usually be carried out without difficulty. The general state of health and any previous illnesses of the patient are also important. Long-term satisfaction can be achieved through follow-up care in around 90 percent of patients.
You can do that yourself
Patients with the tarsal tunnel syndrome sometimes suffer from severe pain in the area of the diseased foot. The associated restrictions in the mobility of those affected often lead to a temporary decline in quality of life.
In order to reduce these complaints in a conservative way and through self-help measures, patients with tarsal tunnel syndrome first discuss the options available with their orthopedic surgeon. Usually, those affected are given special insoles for the shoes that are supposed to relieve the strain. The patients treat the severe pain with drugs prescribed or recommended by their doctor. In order to support the healing process, people with tarsal tunnel syndrome temporarily refrain from sporting activities. In addition, if possible, they reduce the physical strain they may be exposed to at work.
If the conservative measures do not bring about any improvement, surgery is usually the method of choice. Take special care before and after this operation. After the operation, the patients take a few days off work and use the walking aids to relieve the operated foot. Together with their orthopedic surgeon, those affected discuss measures to effectively prevent recurrence of the tarsal tunnel syndrome. This also includes adapting the usual sporting activities.


.jpg)










.jpg)