In the Vulvodynia Patients suffer from abnormal sensations or even pain in the area of the vula that cannot be attributed to external causes. In addition to nerve irritation, triggers can be depression, skin diseases and infections with bacteria or fungi. Treatment is done depending on the primary cause.
What is vulvodynia?
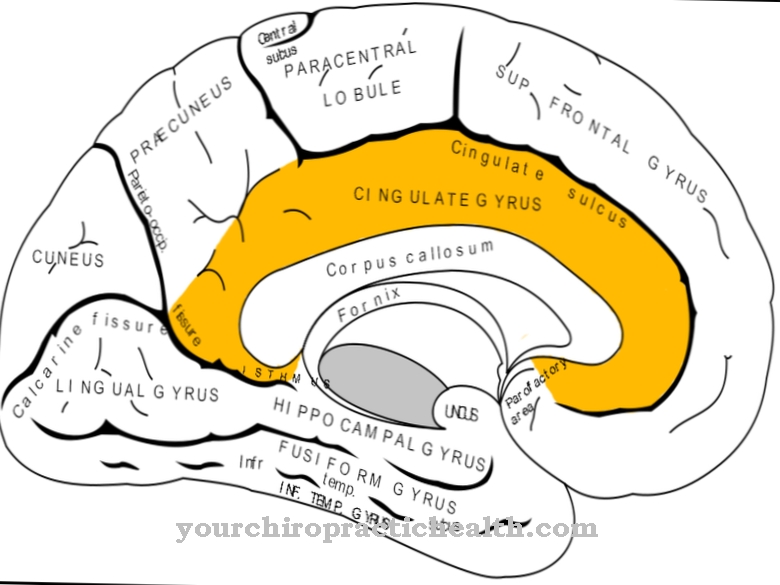
The vulva is all of the woman's external primary sex organs. The vulva can be subdivided into the mons pubis, the labia, the clitoris and the vaginal vestibule. This vulva is made of pubic hair as soon as puberty has set in. As in all skin and mucous membrane areas, there are different mechanoreceptors, temperature receptors and pain receptors in the vulva.
These sensory cells permanently project stimuli to the central nervous system. In this way, sensations such as touch, pain or heat and cold stimuli can be perceived in the area of the vulva. In the Vulvodynia or Vulvodynia Parasitic sensations up to and including painful states occur on the vulva.
These abnormal sensations can extend over the entire area of the external primary sexual organs and be of varying severity. As with all other abnormal sensations, vulvodynia are probably also based on neurogenic causes. The type of discomfort can vary significantly and range from a slight burning sensation to severe pain.
causes
General nerve irritation or neuropathies of nerves in the vulva area can theoretically be responsible for vulvodynia. In practice, the cause of vulvodynia remains in most cases permanently in the dark. The development process has not been conclusively clarified, but in the cases documented so far it is less attributed to skin reactions.
In individual cases, the abnormal sensations were explained by fungal infections, condylomas or general irritation of the skin. The irritation can be caused, for example, by soaps, care products or intimate care products. Hypersensitivity to food ingredients was apparently responsible for the irritation more rarely.
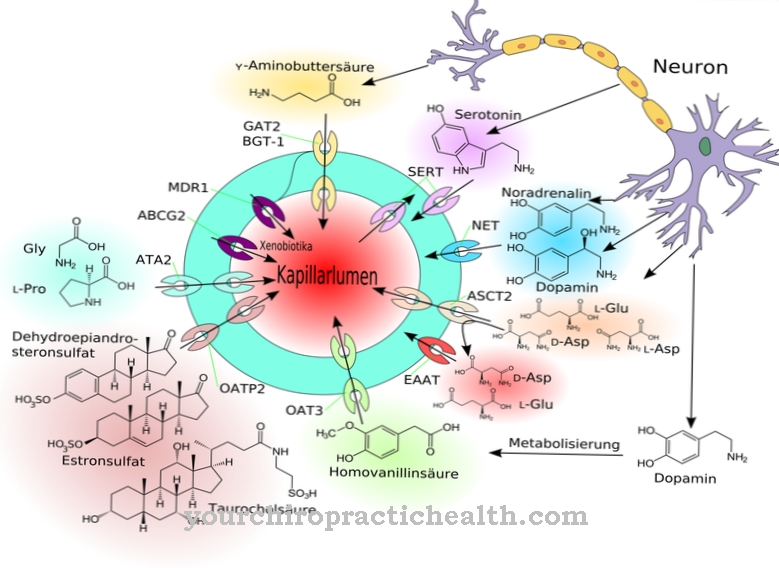
Overreactions to certain histamine liberators in particular have been linked to the phenomenon. In this context, consuming meals containing oxalate and glutamate induces mast cells to release histamines. These histamines mainly cause sharp pain around the vulva. An extremely rare cause of vulvodynia is atopic dermatitis in the vulva area.
Symptoms, ailments & signs
In vulvodynia, the smallest touches in the area of the vulva cause unpleasant irritation and abnormal sensations. Many patients complain, for example, that touching normal underwear or clothing causes pain. Vulvodynia can vary in severity.
Often the discomfort is simply a burning sensation. In some cases, severe pain is also reported. Parasitic sensations in the external primary sexual organs not least affect the intimate life of those affected. Tender touches in this area can lead to unpleasant sensations. In the worst case, the patients develop a general aversion to intimacy due to the unpleasant sensations over time.
In order to prevent such consequences, a quick visit to the doctor is essential. The symptoms that accompany vulvodynia depend on the primary disease. Fungal diseases can, for example, manifest themselves clearly on the skin of the affected area and, in addition to the abnormal sensations, also cause itching. In addition to physical causes, mental illnesses such as depression can also lead to abnormal sensations.
Diagnosis & course of disease
Often women with vulvodynia hesitate for a long time to see a doctor. They are ashamed of their abnormal sensations and are reluctant to bring the problem to doctors because of its location in the genital area. The diagnosis often takes place late. In most cases, the doctor makes a diagnosis of exclusion as part of the diagnosis.
This exclusion diagnosis includes tests for infections such as fungi, bacteria and condylomas. A tissue sample can be taken under a colposcopic view to rule out autoimmune diseases in the affected tissue. The anamnesis also plays a decisive role in the diagnosis.
Depending on whether the patient describes the pain as dull, radiating, stabbing, localized, wandering, pulsating, constant, time-dependent, cycle-dependent or stress-dependent, individual causes may appear more obvious or less likely. Visual diagnostics, which allow the doctor to identify any redness or swelling, is also important. The prognosis depends on the cause.
Complications
Depending on the cause, vulvodynia can have various complications. At first, the abnormal sensations are accompanied by increasing discomfort, combined with painful itching and sometimes with bleeding. If the symptoms are based on depression, mood may deteriorate further as the disease progresses.
There is also the risk that further mental illnesses will develop and further reduce the patient's well-being and quality of life. If an autoimmune disease is the cause, there are usually other symptoms such as chronic rashes, gastrointestinal problems or even muscle paralysis and permanent sensory disorders. Complications increase as the disease progresses and eventually lead to chronic health problems.
Fungal infections, condylomas and similar triggers can also lead to far-reaching symptoms if there is no adequate treatment. However, complications can also arise during therapy. Prescribed antifungal drugs can cause headaches or nausea. Serious physical reactions are possible in the event of intolerance, allergies or liver diseases.
Anticonvulsants also have risks. This can lead to memory lapses, language disorders and, in interaction with alcohol, life-threatening respiratory depression. Antibiotics occasionally cause headache, muscle pain and skin irritation.
When should you go to the doctor?
If you have vulvodynia, you should definitely consult a doctor. It is a serious disease that definitely needs to be treated by a doctor. There is also no independent healing, so that the person affected is always dependent on professional treatment. The earlier a doctor is contacted about vulvodynia, the better the further course of this disease is usually. A doctor should be contacted if the person concerned suffers from severe pain after touching laundry and clothing.
There is a strong burning sensation and itching. In some cases, this pain can also occur after touching people and has a very negative effect on the person's life. If these symptoms appear over a long period of time and do not go away on their own, a doctor must be consulted in any case. First and foremost, you should consult a general practitioner or a dermatologist. Since vulvodynia can also lead to depression or psychological upset, a psychologist should also be consulted.
Treatment & Therapy
Vulvodynia is treated as causally as possible. The individual treatment steps therefore depend on the cause in each individual case. In order to rule out food hypersensitivity, a two-week diet with less irritating foods is followed. Ideally, this diet can heal the vuvodynia caused in this way.
Antimycotics are given for causes such as the fungal infection. If the infection recurs, a tablet treatment should be used instead of a cream treatment. If the creams are used too often, the ingredients can additionally irritate the skin and cause even more severe sensations. Bacterial infections are treated with a specific antibiotic depending on the type of bacteria.
In extreme cases, if the nerve is irritated, stopping the affected nerve can stop the abnormal sensations. In most cases, however, the administration of anticonvulsants is sufficient, as they reduce the sensitivity to pain and itching. Tricyclic antidepressants are given on a trial basis if no cause can be identified or if the anamnesis seems to suggest psychological disorders.
Autoimmunological causes such as neurodermatitis may require prophylaxis in addition to acute treatment. If the patient has already developed a fear or aversion to any kind of intimacy due to the abnormal sensations, cognitive behavioral therapy can allow a reassessment of intimacy situations.
prevention
Vulvodynia caused by bacterial and fungal attack can be prevented to a certain extent. The best possible hygiene is a prerequisite for this. A clean environment makes it difficult for the microorganisms to colonize.
Aftercare
Depending on the underlying causes of the vulvodynia in the respective patient, the ups and downs of the symptoms may still be detectable for years. Therefore, the affected patient should take special care of her vulva. Soap should not be used for daily personal hygiene because it could be unnecessary irritation. An alternative are pH-neutral cleansing lotions or only warm water.
Tight-fitting clothing could also constrict and irritate the vulva. Targeted pelvic floor training helps women to better localize and compensate for their symptoms. The regional adult education centers usually offer appropriate courses. Women who have had vulvodynia also benefit from a fresh, high-fiber diet as it ensures regular bowel movements.
Constipation, for example, would unnecessarily increase the pressure on the vaginal region and thus the symptoms. Many patients affected by vulvodynia have to regain their sexual excitability. Heat pillows or hot water bottles that relax the abdomen are helpful here. Local self-massages with oil and training with vaginal dilators can restore the sexual feeling.
Body-focused sports such as Pilates or yoga support this process. Membership in a support group may also help. The Förderverein Interstitielle Cystitis MICA (www.ica-ev.de) offers appropriate assistance. This self-help organization is intended for patients with interstitial cystitis, but also takes care of vulvodynia patients.
You can do that yourself
Since the causes of vulvodynia are often unclear or varied, the self-help of those affected also consists in carefully observing their own symptoms and ideally keeping a record of possible triggers. Keeping a pain diary, which also includes daily activities, can help identify a connection between the event and pain.
Due to the lack of clarity, an exchange with other patients can also be helpful. Self-help groups are suitable for this. In addition, the pain can be alleviated with specific pelvic floor exercises. Those affected can do this regularly at home. Breathing exercises and meditation can also help to specifically counteract the pain. It also helps some sufferers to act on the painful part of the body with direct heat or cold, using cold compresses, heat plasters or heat pillows. Even light physical exercise such as yoga, Pilates or Qi-Gong can in some cases help to temporarily reduce pain.
In addition, emphasis should be placed on a balanced diet and a healthy lifestyle. Everyday stress factors should be identified and reduced whenever possible. Conscientious hygiene can also lead to better general well-being.










.jpg)