If the white blood cells are severely damaged as a side effect of a drug, the body's immune system can collapse as a result. This opens the door to both bacterial and viral infections, which in extreme cases can have fatal consequences. One then speaks of one Agranulocytosis.
What is agranulocytosis?

Agranulocytosis is used when the proportion of granulocytes falls below 500 cells per microliter of blood.
Granulocytes belong to the white blood cells and can be found wherever the body comes into contact with pathogens, for example on the mucous membranes. They arise in the bone marrow and are mainly responsible for the defense against bacteria and fungi, so they are crucial for maintaining the immune system.
If no more granulocytes are formed in the bone marrow, for example as a result of taking a drug, there is a strong reduction or even a complete absence of granulocytes in the blood.
Forms of agranulocytosis:
In general, a distinction is made between allergy-related and congenital agranulocytosis. Congenital agranulocytoses are rather rare. One example here is the Kostmann syndrome.
Agranulocytosis caused by drugs, however, is more common, with two types being distinguished here. Type I of allergic agranulocytosis is triggered by drugs. The immune reaction to the drug, in which the granulocytes are damaged, occurs independently of time and dose.
Type II is also called toxic agranulocytosis because the drug causes toxic bone marrow damage. It is characteristic here that type II is both dependent on the dose of the drug and time. The difference between type I and type II is that in type I granulocytes are formed, but these are destroyed. In type II, the production of granulocytes in the bone marrow is prevented.
causes
Unless it is a hereditary agranulocytosis, agranulocytosis can be triggered both by an immune reaction to certain drugs and by toxic influences affecting the bone marrow.
The most common cause of agranulocytosis is an intolerance to certain drugs, which can severely damage the granulocytes. Drugs for which agranulocytosis has been seen commonly include:
- Analgesics, e.g. Metamizole, paracetamol
- Antipyretics, e.g. Phenylbutazone
- Antibiotics, e.g. Metronidazole, penicillin
- Neuroleptics, psychotropic drugs
- Thyreostatics, e.g. Thiamazole, carbimazole
- Sulfonamides
- Others, e.g. Antihistamines, antidiabetic drugs
Drugs that cause type II agranulocytosis directly damage bone marrow cells. An example of such a drug is chlorpromazine. It should be noted that the drug causing agranulocytosis can be used again in a correspondingly low dose over time without causing such a reaction. This is different with type I. Here the allergic reaction usually lasts for a lifetime and even the smallest amounts of the drug lead to agranulocytosis again.
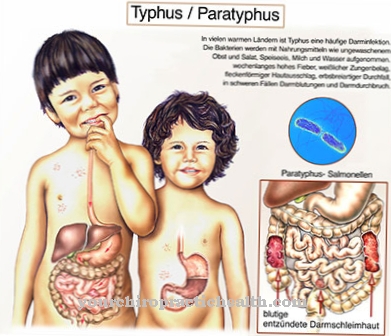
Symptoms, ailments & signs
Agranulocytosis initially manifests itself through unspecific symptoms. At the onset of the disease, headache and muscle pain, fever and general malaise appear. As the disease progresses, it can lead to a high fever with chills and gastrointestinal complaints. Nausea and vomiting are typical, in later stages diarrhea is usually added.
The loss of fluid can lead to deficiency symptoms, which are noticeable in the form of dizziness, tiredness and reduced physical and mental performance. Agranulocytosis can also cause swelling of the lymph nodes, necrosis of the mucous membrane in the mouth and throat and infections of the respiratory tract. The anus area can also become inflamed, which manifests itself in severe pain, itching and bleeding.
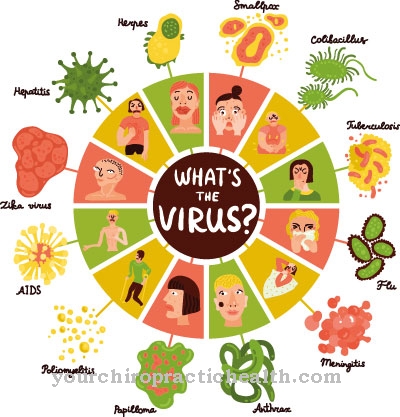
The weakened immune system can no longer fend off any pathogens, which leads to more infections. The mucous membranes are particularly affected - this can lead to herpes or tonsillitis. If agranulocytosis is based on an immune reaction to a drug, the symptoms mentioned appear immediately after ingestion.
Toxic agranulocytosis, on the other hand, is insidious and only causes major symptoms in the later stages of the disease. An external characteristic of those affected is pale skin, which is sometimes associated with sweating and skin irritation.
Diagnosis & course
The onset of agranulocytosis initially manifests itself unspecifically with general malaise, headache and muscle pain and fever. This is followed by a high fever with chills, nausea, swelling of the lymph nodes, as well as necrosis of the mucous membrane in the mouth and throat, infections of the respiratory tract and the anus area. Pneumonia or diarrhea can also occur. Generally there is a severe feeling of illness.
As the immune system collapses, infections in particular occur, especially of the mucous membranes. Examples of this are herpes or tonsillitis.
If it is an immune reaction to a drug, the symptoms appear immediately, often after the first dose. In the case of toxic agranulocytosis, the first symptoms can only be recognized after weeks.
The question of whether or not agranulocytosis is present can be answered very easily by examining the granulocytes in the blood (blood count).
In addition, a physical examination is carried out, in which especially lymph nodes and mucous membranes are carefully examined.
The course of the disease and the medication intake are also discussed with the patient. There are no methods by which the triggering drug could be identified. Therefore, it must be thoroughly determined which drug could be the trigger.
Another possibility for diagnosing agranulocytosis is the bone marrow biopsy, in which samples of the bone marrow are taken with a needle and examined.
Complications
Agranulocytosis is an allergic intolerance reaction to certain drugs. It works directly in the bone marrow and causes an acute shortage of granulocytes. These white blood cells are in fact the body's police force and have the ability to destroy pathogens as well as fungi, parasites and bacteria.
If this body's own defense fails, serious complications are the result. The symptom is considered to be a side effect of preparations such as: antibiotics, analgesics, neuroleptics, thyreostatics and cytostatics. Those affected whose physical condition deteriorates after taking the medication described require medical assistance.
In the worst case, there is a risk of mucosal necrosis or a life-threatening toxic reaction. A thorough medical history can analyze sensitivity, but not cure it. If patients are subject to long-term medication that causes agranulocytosis, they are subject to regular medical checks.
In addition to making a diagnosis, attempts are made to stabilize the patient's immune system. In some cases, the person affected is isolated if symptoms similar to an infection with fever are already evident and the lymph nodes are swollen. A broad spectrum antibiotic is given to restore physical equilibrium.
Depending on the condition, the affected person is given an indication of granulocyte growth factors. In order to minimize the risk of complications, agranulocytosis patients should, in addition to the therapeutic measure, attach importance to accurate hygiene of all body orifices. Due to the increased risk of infection, places where crowds of people come together are avoided.
When should you go to the doctor?
The agranulocytosis must definitely be examined and treated by a doctor. If treatment does not take place, the patient may die in the worst case. For this reason, a weakened immune system must definitely be treated and strengthened again. The person concerned should then see a doctor if there is a fever and general fatigue. This can indicate agranulocytosis. Not infrequently there is also a bad and putrid bad breath and very strong headaches.
These complaints can also indicate the disease. If a visit to the doctor is not possible, an emergency doctor can be called if, for example, there is difficulty breathing or the patient loses consciousness. Pneumonia can also be a symptom of agranulocytosis. Treatment can usually be provided by a general practitioner.
Should there be any further complaints, these can be treated by a specialist doctor. As a rule, agranulocytosis does not reduce life expectancy. A doctor must also be consulted if the agranulocytosis is triggered by a specific drug. However, discontinuing or changing the drug should only be done after consulting a doctor.
Doctors & therapists in your area
Treatment & Therapy
If agranulocytosis is suspected, the offending drug must be discontinued immediately. If it is unclear which medication is involved in a specific case, all medication that is not absolutely necessary must be stopped. The production and number of granulocytes in the blood then increases again and is regulated. The growth can be supported by the administration of granulocyte growth factors.
In order to help the body's own defense system, antibiotics should be taken in the event of infections and fever. The rapid administration of a broad spectrum antibiotic can usually prevent the fatal effects of the disease caused by sepsis.
Hospitalization is required if severe symptoms occur. In order to minimize the risk of infection, it makes sense to isolate the person concerned. In general, special personal hygiene must be observed and crowds of people are avoided due to the increased risk of infection.
Since agranulocytosis is a rather rare disease, many doctors and pharmacists underestimate the risk. Since some triggering drugs are used precisely for the initial, flu-like symptoms of agranulocytosis, a downward spiral can arise when administered.
Therefore, if the symptoms mentioned above occur, it is essential to consult a doctor instead of countering the symptoms with self-medication or by selling an influenza drug through the pharmacist. If the diagnosis is missing or delayed by the doctor, the diseases caused by agranulocytosis can be life-threatening.
Outlook & forecast
Agranulocytosis can be treated well if detected early. However, the symptoms such as fever, nausea, chills, malaise and loss of appetite are so unspecific that the critical death of the granulocytes as part of the leukocytes is often not discovered in time. Rather, other causes for these symptoms are often initially suspected.
Patients taking medications such as certain neuroleptics or analgesics are potentially at risk. If someone has symptoms of long-term flu, the white blood cells in the blood should be measured. If their number reaches a critical lower limit, there is agranulocytosis. This can lead to a complete collapse of the immune system and be fatal. However, agranulocytosis is rare.
Therapeutically, all drugs that can trigger agranulocytosis are discontinued. The number of leukocytes then rises again quickly. In addition, drugs are used that temporarily take over the functions of the immune system until it has stabilized again. The chances of recovery are then good.
Because the symptoms of agranulocytosis are so unspecific, patients who take drugs such as the neuroleptic clozapine should have their blood checked regularly. If the number of leukocytes is continuously checked, action can be taken quickly. If left untreated, agranulocytosis is very difficult in most cases.
prevention
It is important to be aware of the problem of self-medication. Taking medication on its own can lead to serious illness in the event of hypersensitivity to any of the ingredients. Therefore, any medication intake should be discussed with a doctor in advance.
If drugs that trigger agranulocytosis are administered, serious consequences can be prevented with regular blood checks of the person concerned.
If there is agranulocytosis, particular attention must be paid to appropriate personal hygiene, especially in the areas of the mouth, throat and anal region, in order to rule out any risk of infection.
Aftercare
As a rule, the options for follow-up care for agranulocytosis are severely limited. The patient is always dependent on medical treatment. Without treatment, in the worst case scenario, the affected person can even die. An early diagnosis and treatment always have a very positive effect on the further course of the disease and can prevent further complications.
With agranulocytosis, the patient is dependent on taking medication. These should be taken regularly. Possible interactions with other drugs must also be considered. Parents must also ensure that their children take the medication regularly. However, if the agranulocytosis shows severe symptoms, a stay in a hospital is necessary.
The person affected should be careful to take it easy so as not to unnecessarily burden the immune system. For example, the person concerned should not be in high-risk areas. In general, a healthy lifestyle also has a positive effect on the course of agranulocytosis. Above all, a healthy diet and abstaining from nicotine and alcohol can alleviate the symptoms. Contact with other agranulocytosis sufferers is also recommended.
You can do that yourself
In agranulocytosis, the most important self-help measure is to carefully observe the effects of the prescribed medication and to report the results to the responsible family doctor or cardiologist. Switching to another drug is often enough to correct the decrease in granulocytes. Occasionally, however, side effects and interactions occur, which can lead to other complaints.
Patients should also follow a healthy diet that supports the production of white blood cells. Foods rich in vitamin B12 and folic acid, such as bananas, nuts and low-fat fish, have proven particularly useful. An adapted diet and medication are usually sufficient to reduce the agranulocytosis and ultimately to remedy it.
Since the condition can also cause physical and psychological complaints under certain circumstances, depending on the symptoms, further therapeutic measures may be necessary, which the patient can often support by rest and rest. The most important self-help measure in agranulocytosis is to pay attention to the body's own signals. If a lack of granulocytes shows up again, for example due to tiredness or fatigue, a visit to a doctor is recommended.