Andrology is the medical science of Men's medicine and includes the physiology, anatomy and pathology of male reproduction. Andrology also deals with endocrinological and sexual therapeutic aspects and the problems of aging men.
What is andrology?

Andrology, as a study of the male reproductive organs, also deals with their pathology and disorders in all phases of life and in all ages. Different focuses in research and teaching are in the foreground of andrology as a branch of medicine. Andrologists are mostly urologists who specialize in men’s medicine.
The andrological consultation is mainly about disorders of the fertility of men, infertility. In addition, testicular function disorders such as hypogonadism, so-called erectile dysfunction, questions about male contraception and aspects of sexuality in old age play a role.
Findings from andrology play just as important a role in caring for childless couples as they do from gynecology. In reproductive medicine practices, gynecologists and andrologists therefore always work together, because an unfulfilled desire to have children is often due to the inability of men to conceive, which can have very different causes. Andrology is always open to cooperation and collaboration with other medical disciplines. Because without this overall medical perspective, adequate treatment, not only of fertility disorders, is often not possible.
Treatments & therapies
The range of treatments in the medical field of andrology is tailored to the needs of men and their reproductive organs. In particular, hormonal and psychosocial aspects also play an important role in diagnosis and therapy. Because by no means all disorders of male reproduction are actually of organic origin.
This is evidently evident in what is known as erectile dysfunction, from which up to every third man over 50 years of age in western industrialized nations suffers. With age, the production of the male sex hormone testosterone decreases in the testes. Even with the appropriate sexual stimulus, an erection often fails to occur. In younger patients with erectile dysfunction, however, the underlying cause is mostly psychological. At the same time, the experience of orgasm or the process of ejaculation itself can be disturbed.
The treatment of erectile dysfunction often takes a longer period of time and often also includes psychotherapy over several years, which can also include the partner. The andrologist is also the first point of contact for men when it comes to questions of male contraception. The procedure of choice is cutting the vas deferens, known as a vasectomy.
This is usually a reversible intervention, so fertility can be regained at a later point in time by moving back. A common andrological disorder is hypogonadism. Testosterone formation is disturbed by malformation of the testicle, which can have far-reaching effects on mood, libido, cognitive functions and bone metabolism. Male newborns with undescended testicles, i.e. abdominal or inguinal testicles, have a particularly high risk of hypogonadism and the associated infertility.
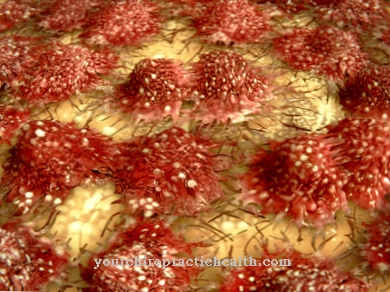
A testosterone deficiency can today be largely remedied with substitution therapy using tablets or gel. However, testosterone replacement therapy is no longer the first choice for testosterone deficiency because of the significantly increased risk of carcinoma. Malignant neoplasms of the urinary and genital organs are also diagnosed and treated by andrologists. For older men, the issues of male fertility are no longer in the foreground, but diseases of the prostate gland, the prostate. If prostate cancer is detected too late, if left untreated, it can lead to death through metastasis, so andrology also plays an important role in prevention.
You can find your medication here
➔ Medicines for potency and erection problemsDiagnosis & examination methods
Doctors for men’s medicine, andrologists, like every other medical specialty, have the entire diagnostic outpatient and inpatient spectrum at their disposal. In the context of urological andrology and reproductive medicine, however, some specialist diagnostics are used. The most important andrological diagnostic and examination procedures include imaging procedures and hormone tests of the blood.
At the first contact between the patient and the andrologist, an ultrasound examination of the testicles and epididymis is typically carried out after the anamnesis. With a special ultrasound head, tissue structure and tissue changes in the testes can be quickly identified and, if necessary, carried out for an extended diagnosis. A blood test may be done in parallel to determine testosterone levels and other important hormones such as DHEA. A urine status is also part of the standard examination in the andrological consultation hours.
This is the best way for the andrologist to diagnose inflammatory changes in the area of the lower urinary tract. In order to better limit a fertility disorder, andrology often uses the so-called spermiogram as an in vivo diagnostic tool. In the man's ejaculate, the number and motility of the sperm cells present are examined under a light microscope. In addition, the ejaculate can also be examined for its chemical-biological composition.
In reproductive medicine, it is also possible to deep-freeze the sperm cells obtained in liquid nitrogen at -196 degrees Celsius in a sperm bank for later artificial insemination. If testosterone replacement therapy is carried out due to hypogonadism, the early detection of contraindications is one of the tasks of the andrologist. For special andrological questions, human genetic examination methods are also used. Many so-called chromosome aberrations can not only lead to reduced fertility, but also to an underdevelopment of the primary and secondary male sexual characteristics.
Over-the-counter fertility test for men
Get information here:
- How good is your sperm? - Take a fertility test at home






















.jpg)

.jpg)
