Abdominal angina is the pain associated with a circulatory disorder in the intestine, which is usually caused by arteriosclerosis of the supplying blood vessels. It usually occurs as a diffuse abdominal pain immediately after eating and can therefore be a warning signal for an impending mesenteric infarction.
What is abdominal angina?
Angina abdominalis is a symptom of a circulatory disorder in the abdominal vessels. "Angina" describes the state of pain, "abdomen" is the medical term for the stomach.
Similarly, there is also angina pectoris, which is much better known and describes the chest pain associated with a heart attack. However, the pathological cause behind these two painful events is the same.
causes
The blood supply to the intestine arises from the large main artery and is then distributed via various defined branches to its target locations in the small and large intestinal wall. The blood is needed here especially when there is work to be done: After eating, the intestine is in action, consumes oxygen for active digestion and also needs the blood as a means of transport for the many nutrients in the liver.
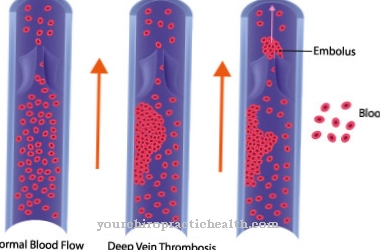
If the intestinal vessels are atherosclerotically calcified and narrowed, this is particularly noticeable after eating: the blood supply has nothing to clog because of the rigid vessels and continues to deliver the same amount of blood as before eating. However, this is no longer sufficient, the intestine does not get enough oxygen and responds with massive pain.
Exactly the same thing happens with angina pectoris and the subsequent heart attack - only the symptoms always occur here when the heart needs a lot of oxygen: when running, climbing stairs, during physical work.
Symptoms, ailments & signs

© Alila Medical Media - stock.adobe.com
The symptoms of angina abdominalis depend on the severity of the circulatory disorders in the abdominal vessels. The disease can be divided into four stages. In stage I there are no symptoms at all. Often it is an incidental finding. If the vessels narrow further, stage II occurs. Here severe abdominal pain can occur after meals.
The greater the amount of food consumed, the stronger the pain. The patient often eats smaller meals to alleviate the symptoms. In stage III the pain persists. Only their intensity fluctuates, which also depends on the amount of food consumed. The fourth stage of angina abdominalis is characterized by an acute abdomen with an often fatal outcome.
If certain intestinal arteries are completely blocked, the affected section of the intestine can no longer be supplied with blood and supplied. Entire loops of intestine then often die off. If action is not taken in time, the intestine breaks through and the contents of the intestine spill into the abdominal cavity. If left untreated, this leads to life-threatening peritonitis.
After the vascular occlusion, the previously existing long-term abdominal pain initially disappears. After about 24 hours there is an acute abdomen, which is characterized by a hardened abdominal wall with defensive tension, fever and a racing heart. Life-threatening complications such as circulatory shock, intestinal paralysis or sepsis can then occur as complications.
Diagnosis & course
The symptom of angina abdominalis can often recur for weeks or months after eating and then disappear again shortly afterwards without anything bad happening at first. Depending on the condition of the blood vessels, progressive calcification and more or less developed collateral supply, damage to the intestinal wall can occur in the long term, which then no longer transports and absorbs the food pulp properly. Malnutrition, constipation, diarrhea and bloody stools can result.
In the worst case, a mesenteric infarction occurs, which, like a heart attack, occurs when the blood supply to the intestinal wall becomes acutely so bad or comes to a complete standstill that the intestinal section that is dependent on it dies.Here you typically have massive pain for a few hours, which then suddenly get better ("lazy peace"), only to return irrevocably a few hours later.
Such a damaged intestine can often no longer be saved even surgically and in a very short time floods the body with toxic and acidic substances, which is often fatal. Massive abdominal pain after eating should therefore lead everyone to the doctor immediately or call an emergency doctor. One should not let the "lazy peace" dissuade one from it either.
Based on the typical symptoms of angina abdominalis, a doctor can make the diagnosis with sufficient certainty. Since arteriosclerosis usually does not only occur in one region of the body but affects the entire body, heart problems, leg pain, increased blood lipid levels, high blood pressure or diabetes are further indications that the abdominal pain is probably vascular-related. Atrial fibrillation can also contribute to the symptoms of the calcified abdominal vessels via blood clots that have been carried over from the atrium.
Complications
If angina abdominalis is not recognized in time, inflammation of the intestinal tissue (ischemic colitis) occurs with permanent abdominal pain, especially after eating. If these are left untreated, an intestinal infarction (mesenteric infarction) can follow. First of all, the patient feels stab-like pain in the intestinal area for a few hours, which returns after a short time.
If no doctor is consulted at this stage, the affected parts of the intestine will begin to irreversibly die. In addition, this stage is often accompanied by inflammation of the peritoneum (peritonitis), which now causes persistent severe abdominal pain. The only help after the onset of the infarction is an immediate operation.
The dead intestinal parts are removed and the blood circulation system of the digestive tract is stabilized. The later this intervention takes place, the lower the probability of promising results. Too long hesitation can lead to an enormous loss of bowel length.
Digestive disorders occur with consequences such as dehydration, lack of nutrients, diarrhea and weight loss. In the worst case, short bowel syndrome occurs. Since abdominal angina is a clinical picture that is triggered by arterial malfunctions, the same patients often suffer from heart attacks or strokes.
When should you go to the doctor?
If pain or pressure in the intestinal tract persists, the doctor or a gastroenterologist should be consulted. The doctor can use the symptoms and a physical examination to determine whether you have angina abdominalis and, if necessary, start treatment immediately. Due to the acute risk of infarction, surgery usually takes place immediately after diagnosis. For this reason, a visit to the doctor should not be postponed.
A visit to a doctor is particularly advisable if symptoms of an intestinal disease keep recurring. Clear warning signs are constipation, diarrhea, and bloody stools. It is also characteristic that severe abdominal pain occurs 15 to 30 minutes after eating. If these complaints occur, the following applies: go to the doctor and clarify the cause.
People with pre-existing conditions such as high blood pressure, high blood lipid levels or diabetes should speak to their doctor immediately if the symptoms mentioned occur. In the case of chronic abdominal pain, the intestinal tissue may already be inflamed and the angina abdominalis must be treated surgically immediately.
Doctors & therapists in your area
Treatment & Therapy
A blood test for acidic metabolic products can acutely confirm the suspicion of a mesenteric infarction or make it unlikely. Analogous to the cardiac catheter examination for chest pain, there is also a radiological contrast agent examination for blood circulation-related abdominal pain, which allows the condition of the blood vessels to be assessed. However, it does not have to be carried out immediately in all cases.
The therapeutic focus of treatment is blood thinning and anticoagulation with ASA or Marcumar. This reduces the likelihood that more clots will form on the already narrowed arteries and completely block the vessel. In the case of an acute infarction, heparin administration, pain therapy and immediate emergency surgery are also necessary.
Outlook & forecast
In many cases, early treatment of abdominal angina cannot take place because the symptoms and symptoms are not particularly clear or characteristic.
In most cases, however, those affected suffer from relatively severe abdominal pain, which mainly occurs after eating and thus significantly reduces the person's quality of life. It is not uncommon for diarrhea or constipation, and thus deficiency symptoms, to occur.
The patient's stool can also be bloody. It is not uncommon for abdominal angina to lead to heart problems and increased blood lipid levels. Leg pain can also occur and be accompanied by diabetes. Without treatment of angina abdominalis, the life expectancy of the patient is significantly reduced and reduced.
The treatment itself can take place with the help of medication and thereby greatly alleviate the symptoms. In some cases or in acute emergencies, surgical interventions are necessary. As a rule, it cannot be predicted whether this will lead to a reduction in the patient's life expectancy. In most cases, a healthy lifestyle with a healthy diet can also have very positive effects on this disease.
prevention
Here, too, prevention is better than aftercare: the risk of arteriosclerosis can be minimized with a healthy lifestyle. That means: No smoking, little alcohol, Mediterranean diet, avoiding stress, doing moderate but regular exercise. High blood pressure and [[diabetes mellitus] as well as increased blood lipids massively increase the risk of hardening of the arteries and should therefore also be avoided or consistently treated.
Aftercare
Abdominal angina may recur after it has healed. Patients do not build immunity. The purpose of follow-up care is to prevent repeated complaints. Those affected bear the main responsibility for this. You have to give up unhealthy habits. Medical check-ups include physical exams and a detailed discussion of symptoms.
Imaging tests like CT and MRI can provide clarity. Usually, the patient turns to their doctor with specific signs. Various behaviors have established themselves as essential means of avoiding abdominal angina, which can be subsumed under the term “healthy lifestyle”. Above all, this means avoiding addictive substances such as nicotine and alcohol. In addition, patients should maintain a balanced diet.
Several servings of fruit and vegetables should be on the daily menu. Physical exercise brings the necessary fitness. Stress in everyday life and at work should be avoided. Successful treatment is not infrequently performed surgically. In the following weeks, follow-up care is aimed at preventing complications.
Patients have to take it easy, so it is essential to plan recovery phases. Food intake should ideally begin with small meals that are spread over the entire day. Depending on the procedure, regular bowel checks may then be necessary.
You can do that yourself
Abdominal angina does not fall within the scope of self-treatment. This disease can develop into a life-threatening condition and requires immediate medical, possibly emergency, care. Measures from the field of self-treatment can only be carried out during or after the operation.
In any case, the body can be supported by consistently avoiding nicotine and alcohol. Those affected should ensure a balanced, high-fiber diet. In particular, the proportion of fruit and vegetables should be increased. This provides the body with important vitamins and minerals. This supports the entire healing process.
A supplementary intake of micronutrients in powder or tablet form can be considered. Basically: everything that supports digestion and blood circulation is helpful. This also includes regular exercise in the fresh air and reducing stress as well as an adequate supply of fluids (preferably still mineral waters or unsweetened herbal teas).
It is imperative to exercise restraint immediately after an operation. Initially, a gradual diet - with several small meals - will have to take place. With timely treatment, patients can live again without major restrictions. If parts of the intestine have to be removed, more attention must be paid to digestion in the future. Elderly people and diabetics in particular - who count as risk groups - should have their intestinal vessels checked regularly. This can be done by your family doctor or an internist.


.jpg)
.jpg)
.jpg)




















