In the Coarctation of the aorta it is a congenital heart defect. There is a narrowing of the main artery.
What is coarctation of the aorta?

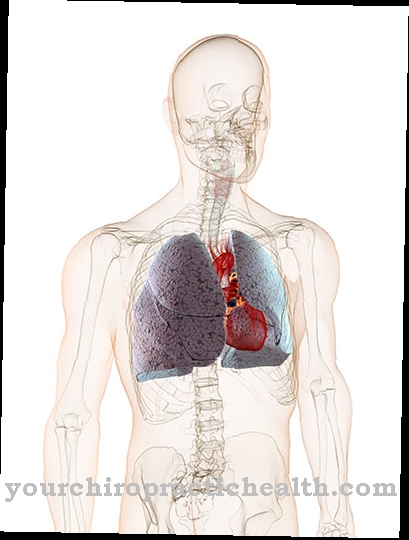
© peterjunaidy - stock.adobe.com Coarctation of the aorta (Coarctatio aortae) is the second most common type of congenital heart defect. It occurs in the region of the aortic isthmus (Aortic isthmus) to a narrowing of the lumen of the aorta (main artery). This stenosis results in an increase in pressure on the outflow tract of the left ventricle. The narrowed main artery increases the resistance.
In order to overcome this, the heart works harder, causing it to enlarge and thicken, which leads to further weakening. The stenosis of the aortic isthmus is congenital and occurs in 7 percent of all heart defects. The malformation occurs more frequently in boys than in girls.
causes
It is not exactly known what causes coarctation of the aorta. There are two theories about how it came about. The first thesis sees a reduction in blood flow in the main artery, which takes place during the embryonic period, as the trigger. The second theory blames dislocated tissue of the ductus arteriosus for the narrowing.
Doctors divide coarctation into two different forms:
- the preductal coarctation of the aorta
- postductal coarctation of the aorta
In the case of preductal coarctation of the aorta, the narrowing is in front of the confluence of the ductus arteriosus. In addition, there is often a tubular underdevelopment of the aortic arch and parts of the descending aorta. It is not uncommon for a ventricular septal defect to occur. For most of those affected, the severe coarse aorta prevents blood flow from the ascending aorta to the descending aorta.
For this reason, the blood supply to the ascending aorta takes place almost exclusively through the pulmonary artery. The venous blood flows through the open ductus arteriosus. As a result, there is a reduced blood flow to the lower body area. However, if the duct is closed, the femoral impulses weaken, which in turn reduces blood pressure.
This increases the risk of anuria and kidney failure. In the postductal form, which is less common, the stenosis of the aortic isthmus is located behind the mouth of the duct in the direction of the artery. The narrowing of the lumen is similar to an hourglass.
Symptoms, ailments & signs
The type of symptoms and the time of their occurrence depend on the location of the coarctation of the aorta and its severity. In the case of preductal coarctation of the aorta, even newborn children suffer from a lack of oxygen and heart failure. This is noticeable through poor drinking, failure to thrive and cyanosis, in which the skin and mucous membranes turn bluish.
Hegatosplenomegaly can also occur, in which the spleen and liver enlarge at the same time. It is a mixture of hepatomegaly and splenomegaly. If there is an occlusion of the ductus botalli, there is even a mortal danger. Without timely treatment, the death rate of sick children is 90 percent.
Postductal coarctation of the aorta is more difficult to diagnose, as only a heart murmur and a difference in pulse can be heard during preventive examinations. Toddlers are often affected by nosebleeds, calf pain during exercise, cold feet and headaches. In adolescents, however, there is a risk of intermittent claudication.
Diagnosis & course
The doctor can usually diagnose coarctation of the aorta by listening to a heart murmur. This occurs along with a difference in blood pressure between the upper and lower limbs. While there is high pressure in the arms, the pulse and blood pressure in the legs are rather weak. An echocardiogram (EKG), an X-ray examination, an angiography or a magnetic resonance tomography (MRT) can be carried out as further examination measures.
Precise examination results are possible with the help of a cardiac catheter examination. Doctors push a tube to which a measuring device or camera is attached to the heart. In this way they assess the structure of the aorta, the blood pressure conditions and the blood flow.
If the coarctation of the aorta can be eliminated, the affected children can normally be completely stressed again and are considered cured. However, they will have to have cardiologist checkups for the rest of their lives. Bulging in the aortic wall are possible long-term complications.
Complications
Complications that can arise in connection with untreated coarctation of the aorta (ISTA) depend on the exact location of the congenital stenosis and the type and severity of the obstruction. If the stenosis is still in front of the botallus duct, the possible complications are particularly serious because the body cannot form any alternative blood vessels (collaterals).
Serious complications then arise in newborns due to an insufficient supply of oxygen and nutrients to the lower half of the body and the internal organs such as the kidneys, liver and intestines. Severe neonatal jaundice can develop as a visible complication. As a further complication, shock symptoms with over-acidification of the blood can develop.
The pH value can drop below seven, which usually leads to irreversible brain damage. In less serious cases of ISTA, there are hardly any complications in newborns because a network of collaterals has formed that takes over a large part of the blood supply. In many cases, the disease initially goes unnoticed and only becomes noticeable in childhood or adulthood.
If an ISTA goes unnoticed and therefore goes untreated, permanent high blood pressure can develop because the aorta function is greatly reduced. In these cases, the body tries to compensate for the impending decrease in diastolic pressure by increasing systolic pressure. The multitude of complications that can result from this correspond to those of arterial hypertension.
When should you go to the doctor?
A decisive factor in the symptoms of coarctation of the aorta (ISTA) is the exact location of the narrowing of the main hit (aorta). It can lie immediately in front of or behind the ductus arteriosus, which short-circuits the pulmonary circulation with the body circulation before birth. If the stenosis is in front of the short-circuit window (preductal), the left heart is heavily stressed and also overloaded. As a rule, the symptoms are so severe that the newborn must already be treated surgically because it is a life-threatening condition.
If the constriction of the aorta is located directly behind the confluence of the ductus arteriosus (postductal), alternate vessels (collaterals) can usually form across various thoracic arteries. In many cases, a postductal ISTA therefore goes unnoticed until adulthood. The decision as to whether to see a doctor is only made once the disease has been diagnosed by chance. If coarctation of the aorta was only discovered and diagnosed in adolescence or early adulthood, the further procedure should be made dependent on how well the collateral circuits can compensate for the constriction in the aorta.
The systolic pressure differences between the upper body and the lower body, for example between the arm artery and leg artery, indirectly provide a measure of the “quality” of the compensation. The smaller the pressure differences, the better the collaterals work. For a long-term prognosis, it is recommended that an angiologist or cardiologist check the size and course of the collaterals.
Doctors & therapists in your area
Treatment & Therapy
For both preductal and postductal aortic coarctation, medical treatment is necessary as early as infancy. Without appropriate therapy, the mortality rate is 60 to 90 percent. If serious symptoms occur, it is considered a medical emergency that requires immediate surgery. Because the heart does not have to be surgically opened, a heart-lung machine can usually be dispensed with.
During the procedure, the surgeon will make an incision on the left side of the chest between two ribs. The aorta is clamped in front of and behind the stenosis during the operation. If the narrowing is short, the diseased blood vessel area can be removed. The surgeon then sutures the ends of the vessels together.If, on the other hand, there is a longer narrowing, the lower section of the blood vessel can be sewn to the aortic arch.
Parts of the left arm artery are sometimes used for the reconstruction. As an alternative to surgery, balloon dilatation can be performed to treat coarctation of the aorta. The constriction is widened with the help of a balloon catheter. However, there is then the risk that a narrowing will occur again. For this reason, surgery is usually preferred. If re-stenosis occurs after an operation, balloon dilatation is considered more suitable.
Outlook & forecast
Coarctation of the aorta does not always have to lead to a reduced life expectancy or other symptoms. However, those affected depend on therapy to relieve the symptoms and prevent further complications.
As a rule, the children have to be supplied with oxygen immediately after birth, as otherwise the newborns would die. Children can suffer from a developmental disorder. Unfortunately, it is not always possible to limit this disruption. In severe cases, the patient's skin can also turn blue. If left untreated, the disease can also lead to an enlarged liver or spleen, so that the patients in these regions suffer from severe pain. Furthermore, coarctation of the aorta can lead to nosebleeds and severe headaches in everyday life.
If the disease is not treated, it can significantly reduce the patient's life expectancy. However, the symptoms can be alleviated very well by treatment, so that the person affected can fully participate in everyday life. Usually only a few further examinations are necessary after a successful treatment.
prevention
Coarctation of the aorta is a congenital disease. Therefore there are no effective preventive measures.
Aftercare
Since coarctation of the aorta is a congenital disease, it cannot be treated causally, but only symptomatically. Complete healing cannot be achieved, and the options for aftercare for coarctation of the aorta are relatively limited. The patient is dependent on medical treatment, as otherwise the person concerned may die prematurely.
If the acute symptoms of aortic coarctation occur, an emergency doctor must usually be called directly or the hospital visited. The earlier coarctation of the aorta is diagnosed and treated, the higher the probability of a positive course of the disease. After the surgical procedure, the person affected has to take care of his body and rest himself.
In doing so, strenuous activities or sporting activities are to be avoided. Stress should also be avoided. Also the intake of nicotine and alcohol should be done in the lowest possible degree. In general, a healthy lifestyle with a healthy diet has a positive effect on the course of the disease. If the doctor prescribes medication for the patient with coarctation of the aorta, attention must be paid to taking these medications regularly. Interactions with other drugs must also be considered.
You can do that yourself
Priority in the therapy of coarctation of the aorta are consistently implemented prophylactic and therapeutic measures. Thanks to advances in diagnostics, we now know the effectiveness of careful cardiological monitoring and care. Care should be provided in a center that is experienced in dealing with congenital heart defects.
The disease is often accompanied by increased blood pressure. In addition to drug therapy, all antihypertensive aids are welcome - provided they do not burden the patient too much. There are two things that help lower blood pressure: diet and exercise.
With regard to nutrition, almost all studies indicate a connection between salt consumption and high blood pressure. Patients who reduce the amount of salt in their diet or who pay attention to the salt content of finished foods can have a considerable positive influence on their blood pressure values.
In order to permanently lower blood pressure values, consistent and regular exercise is necessary. Only a few exercises have no effects, on the contrary, they put a strain on the body, which is susceptible anyway. Sports that lower the blood pressure are all those in which the patient strengthens or improves stamina and stamina. These include walking, running, cycling and swimming. Avoid contact sports or so-called stop-start sports such as tennis; Sports with high static loads such as weightlifting, gymnastics or rowing should also be viewed critically.



.jpg)




















.jpg)


