The Superior mesenteric artery syndrome is a compression syndrome that leads to upper abdominal pain, difficult food intake and nausea and even vomiting. The patients often suffer from malnutrition, which those around them often mistake for the consequences of an eating disorder. The treatment is mostly invasive and consists of decompression that allows normal food intake again.
What is Superior Mesenteric Artery Syndrome?

© tigatelu - stock.adobe.com
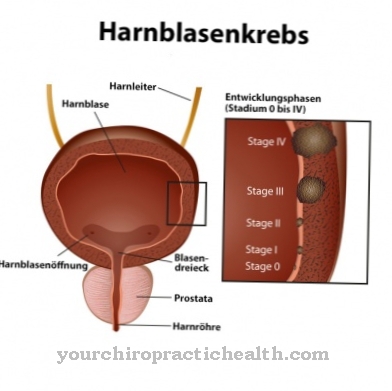
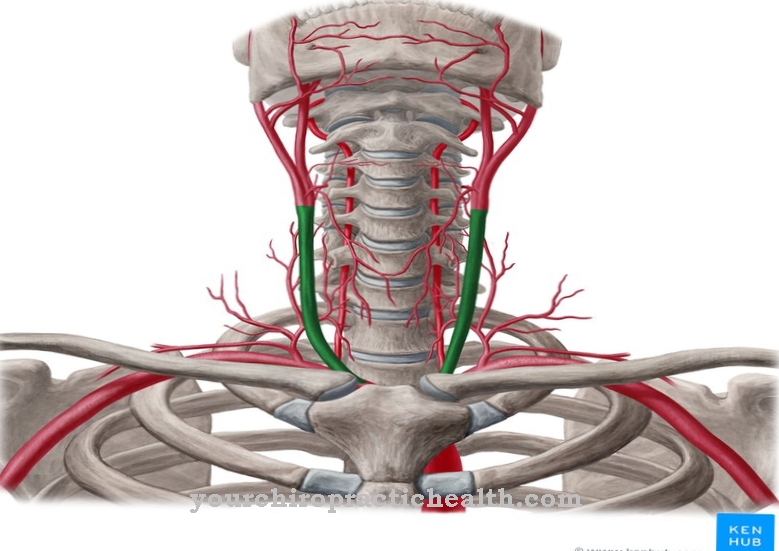
The superior mesenteric artery is better known as the superior visceral artery. It is a branch of the aorta that arises behind the pancreatic neck between the renal arteries and the trunk of the celiac trunk. The origin lies somewhat at the level of lumbar vertebrae 1. The arterial vessel can be affected by various vascular diseases.
One of them is the so-called superior mesenteric artery syndrome, also known as Wilkie syndrome, Upper mesenteric artery syndrome, Duodenal compression or acute gastroduodenal obstruction is known. The names are also common synonyms mesenteric duodenal compression syndrome, Mesenteric root syndrome and chronic duodenal lilus.
The gastrointestinal vascular disease leads to duodenal stenosis, which takes place on the basis of compression in the area of the distal duodenal segment. This area lies between the superior mesenteric artery and the aorta. The main age of onset of the syndrome is between the ages of ten and 39. The prevalence is estimated at 0.3 percent in the normal population. Women are affected far more often than men.
causes
The superior mesenteric artery syndrome is caused by compression of the distal duodenal section between the superior mesenteric artery and the aorta. This compression takes place most often in the course of operations. At this point, especially scoliosis operations should be mentioned, after which the syndrome is said to occur in about 2.4 percent of patients.
In addition, chronic weight loss appears to be a risk factor for compression disease. Accordingly, the syndrome is frequently observed in the context of nutritional disorders. Additional risk factors include anatomical anomalies and pathological body processes with a local limitation.
All of the above-mentioned risk factors have one connection in common, which can be described as the primary trigger of the superior mesenteric artery syndrome. The physiological angle between the aorta and the superior mesenteric artery is between 38 degrees and 56 degrees. If the angle between the two vessels decreases to six to 25 degrees due to the risk factors mentioned here, compression in the sense of the superior mesenteric artery syndrome is to be expected.
You can find your medication here
➔ Medicines for stomach ailments and painSymptoms, ailments & signs
The superior mesenteric artery syndrome is associated with some clinically typical symptoms. For example, those affected often complain of pain in the upper abdomen, which tends to occur after eating. In addition, the patient experiences a feeling of fullness that is subjectively felt to be rapid, which can lead to weight loss.
In some of the documented cases, those affected even showed signs of malnutrition. Because of the pain felt after eating, many of those affected often avoid eating and develop a real fear of eating. Symptoms such as nausea and vomiting were observed in individual cases.
For this reason, the externally apparent symptoms of the superior mesenteric artery syndrome often resemble an eating disorder. To observers, it can appear as if the patient is sick with vomiting or a similar disorder. Overall, the superior mesenteric artery syndrome is associated with rather unspecific symptoms.
Diagnosis & course
Since the superior mesenteric artery syndrome has relatively unspecific symptoms and is extremely rare, it is often difficult for the doctor to make a diagnosis. In many cases, the patient's complaints are traced back to a psychological cause over a long period of time, dismissed as an addictive disease or mistaken for other eating disorders.
This connection is made more difficult by the fact that most of the patients with the syndrome are women. If a diagnosis takes place, imaging procedures usually provide information as part of this diagnosis. The causal compression can be localized and identified via the imaging. It often takes at least a few months before imaging is initiated. Many doctors are too unfamiliar with the syndrome to consider it.
Complications
The superior mesenteric artery syndrome has some clinical symptoms that clearly indicate the presence of this compression disorder. Those affected suffer from a congenital or acquired narrowing in the area of the duodenum between the upper intestinal artery and the main artery. This narrowing is the cause of various health disorders that severely limit the quality of life of those affected.
The patients complain of upper abdominal pain, nausea, vomiting and difficulty in eating. This gastrointestinal vascular disease leads to a rapid feeling of satiety, which can cause visible weight loss and malnutrition over a longer period of time. Because of the severe pain in the upper abdomen that occurs immediately after eating, many sufferers avoid eating or develop real fear of it.
Since the superior mesenteric artery syndrome is associated with rather unspecific symptoms, eating disorders or addictive behavior are suspected in many cases. A differential diagnosis and the associated individual treatment are therefore delayed in many patients, which makes the complications and symptoms worse.
With appropriate treatment, the prognosis is positive, because the compression syndrome can be remedied without risk through an invasive procedure. However, many patients develop postoperative psychosomatic complications if the disease has existed for a long time. This abnormal behavior manifests itself as an increased fear of food which caused excessive pain prior to surgery. However, these anxiety states can be successfully treated with professional psychological support.
When should you go to the doctor?
The superior mesenteric artery syndrome should definitely be evaluated and treated by a doctor. This disease does not self-heal and, in the worst case scenario, the patient can be killed if treatment is not initiated.
A doctor should be consulted if the ingestion of food is refused due to severe pain in the abdomen. The patients can also suffer from a fear of eating and have symptoms such as vomiting or nausea. In the case of superior mesenteric artery syndrome, a doctor should be consulted, especially in the event of refusal to eat.
It is not uncommon for the symptoms to resemble an eating disorder. As a rule, the treatment should be initiated by a family member, as the patients themselves often cannot admit the complaint. In the case of psychological complaints in particular, urgent treatment is necessary so that the malnutrition does not lead to further complications or consequential damage.
In severe cases, the affected person must then be fed artificially through a gastric tube. In particular, the parents and partners of those affected must pay attention to symptoms and signs of the superior mesenteric artery syndrome and, in any case, consult a doctor.
Doctors & therapists in your area
Treatment & Therapy
The treatment of the superior mesenteric artery syndrome consists of causal treatment steps and symptomatic treatment measures. The release of the compression is one of the causal therapy steps. This decompression usually takes place as part of an invasive procedure.
The symptomatic treatment steps are aimed at gaining weight. First of all, malnutrition symptoms are compensated for with intravenous supplements. A duodeno-jejunostomy, for example, can be performed if patients cannot manage to eat.
The jejunostomy is a surgical procedure in which a connection is made between the abdominal wall and the upper small intestine. The surgeon places an intestinal tube through the opening to ensure enteral nutrition. Jejunostomies can be performed surgically in the form of an open or laparoscopic operation.Interventional-endoscopic variants of the procedure are also available, for example jejunoscopy.
If the superior mesenteric artery syndrome has persisted for a long time, psychotherapeutic or psychological support can be useful. Often, because of the symptoms, those affected suffer from fear of food intake even after a long period of time. This fear can be countered with professional guidance so that normal food intake is possible again and the rebuilt weight can be maintained in a natural way.
Outlook & forecast
The superior mesenteric artery syndrome has a good prognosis. The difficulty of the disease lies in the diagnosis. The symptoms often confuse the disease and thus delay the start of treatment. If it starts too late, there may already be organ damage or functional disorders. Most of them are irreparable.
The course of the disease is progressive and in severe cases can lead to a breakdown of the system. If medical care is deliberately refused, the patient continues to lose weight. Women are more often affected by the disease than men. Nevertheless, the disease takes the same course in both sexes.
Corrective surgery is carried out within medical care. In this the functionality of the vessel is restored. Then the patient must be cared for for the purpose of controlled weight gain. Within a few months, the sick person can normally be discharged as symptom-free.
A return of the symptoms is considered unlikely. Nevertheless, the experiences can lead to various consequences. Usually psychological problems arise that have to be treated after the physical treatment. A mental disorder is treated in psychotherapy. Symptom relief can take months or years to complete.
You can find your medication here
➔ Medicines for stomach ailments and painprevention
The superior mesenteric artery syndrome can only be prevented to the extent that a reduction in the anatomical angle between the aorta and superior mesenteric artery can be prevented.
Aftercare
In the case of the superior mesenteric artery syndrome, in most cases those affected have only very limited possibilities for self-help. Usually, patients need medical treatment to relieve and limit the symptoms of the syndrome. Complete cure cannot always be guaranteed, and in some cases life expectancy may be reduced as a result of the syndrome.
The superior mesenteric artery syndrome is usually treated by surgery. Although this proceeds without complications, an early diagnosis with timely treatment is crucial in order to prevent further symptoms. After such an operation, those affected definitely need to rest and take care of their bodies.
You should refrain from strenuous activities or sporting activities in order not to unnecessarily burden the body. Any stressful situation should also be prevented. After the procedure, only light meals are allowed. Only over time does the body have to get used to normal food so that the person affected can take on weight again. Furthermore, in the case of the superior mesenteric artery syndrome, contact with other sufferers of the syndrome can be useful, as this can lead to an exchange of information.
You can do that yourself
There are no self-help options for patients to treat the cause of the disorder. However, the disease has been linked to persistent malnutrition. People who suffer from an eating disorder should therefore take countermeasures in good time with regard to the superior mesenteric artery syndrome and, if necessary, start therapy.
If the malnutrition was only triggered by the compression of the intestinal artery, it is important that those affected gain weight again as soon as possible after the operation to eliminate the disorder. However, the weight gain should not result from excessive consumption of unhealthy foods such as prepared products, fatty meat, french fries or sweets.
Instead, those affected should have a nutritionist put together a nutritional plan that enables healthy weight gain. Nuts and seeds, high-quality vegetable fats and oils and whole grain products are beneficial.
If there was a vitamin or mineral deficiency during the illness, these deficits can be quickly compensated for with dietary supplements.
Some patients develop a pathological fear of eating during illness, as eating in the past has been associated with severe pain. If these anxiety conditions persist after the physical causes are corrected, therapy should be considered. In many cases, however, appetite-stimulating agents help to return to normal eating behavior.

.jpg)









.jpg)




.jpg)


