The Arteriogenesis describes the growth of collateral arteries after a stenosis and is to be distinguished from angiogenesis. Factors such as shear forces, vascular dilation and monocyte accumulation play a role in the process. In the future, arteriogenesis induction will presumably enable patients to be bypassed "naturally".
What is arteriogenesis?

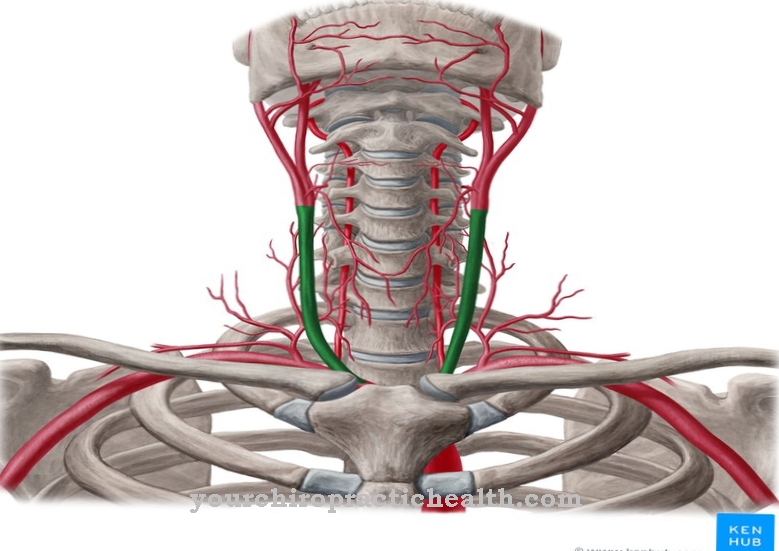
The growth of arteries from already established networks of small arterial connections is called arteriogenesis. In angiogenesis, on the other hand, completely new blood vessels sprout out of old, i.e. already existing blood vessels. Arteriogenesis in the sense of the growth of so-called collateral arteries takes place after larger arteries have been closed, i.e. after stenoses.
The arteriogenesis corresponds to the only physiologically efficient type of blood vessel growth and can compensate for blood circulation deficits. The stimulation of arteriogenesis is incumbent on physical forces, such as the shear stress that exist after stenosis due to the increased blood flow within the collateral arterioles. In addition, monocytes are believed to be stimulating factors. They are the largest immune cells in human blood.
In contrast to the related process of angiogenesis, arteriogenesis takes place completely independently of the oxygen supply and is therefore not influenced by hypoxia in the sense of insufficient oxygen supply.
Function & task
The process of arteriogenesis is initiated with the continuing dilatation of the vessel lumen, which leads to an accumulation of myocytes and hypertrophy of the endothelium. Arteriogenesis is triggered by stenoses that block a supplying blood vessel. The occlusion lowers the perfusion pressure.
At the same time, increased shear forces occur in the remaining blood vessels, which activate the endothelium of the vessel. On the basis of this activation, an inflammatory reaction occurs, in which nitric oxide and transcription factors are released. The most relevant transcription factors include HIF-1α, the hypoxia-induced factor.
The processes described release cytokines, especially MCP-1 or, better, Monocyte Chemotactic Protein-1. In addition, the inflammatory cells are activated, which in addition to the monocytes also include the macrophages. The gene expression of the adhesion molecules, for example intracellular adhesion Molecule-1 and ICAM-1, is induced to a greater extent. During arteriogenesis, the original vessel diameter partially expands to 20 times and in this way enables an adequate blood supply again.
The Max Planck Society points out that arteriogenesis has been associated with the accumulation of monocytes in growing collateral vessel walls in a number of studies. Wolfgang Schaper's research group then investigated the origin of cells and the role that circulating monocytes play in arteriogenesis. In experimental approaches, they increased and decreased the number of monocytes in the animals' bloodstream.
In the first group, they initiated an evacuation of the monocytes from the blood, whereby the blood concentration of the immune cells increased several times over the normal value due to the rebound effect after about two weeks. The group with sustained monocyte depletion showed a significantly lower level of arteriogenesis than the control group after blood flow was restored. The rebound group, however, showed increased arteriogenesis. Through their study, the scientists succeeded in establishing functional relationships between the monocyte concentration in the peripheral blood and the extent to which the collateral vessels grow during arteriogenesis.
Illnesses & ailments
Medical research aims to stimulate arteriogenesis in the future and to offer patients with cardiovascular diseases new therapeutic options in the future. Arteriogenesis could, for example, create a natural bypass flow. The bypass is currently still artificially created as part of an operation and is used to bridge passage obstacles. Bypass surgery creates a connection between the beginning and the end of stenoses.
Most often, this operation takes place on the heart, especially in the case of severely narrowed or completely closed coronary vessels that have to be bridged. The bypass restores an adequate blood supply to the heart muscle.
Bypasses are used in vascular surgery, for example, for the therapy of intermittent claudication in the late stage or for the treatment of aneurysms. In cardiac surgery, coronary artery bypass is a frequently used bypass for coronary heart disease. Veins or arteries are taken from the patient's body or from the deceased and used to bridge the gap. Artificial fabrics such as Gore-Tex or other artificial vascular prostheses are now also used. For example, there is not a sufficiently long vein available for an aortic replacement, so that so-called tubular prostheses are the only therapeutic option so far. As an alternative to bypass, vascular surgery uses implants as grafts and thus replaces the entire vascular section affected by a passage obstacle.
As research advances and research into arteriogenesis continues, an entirely new and completely natural option for treating obstructions to passages may emerge. Passage obstacles are a relevant topic, especially in the western world, as diseases such as arteriosclerosis have already developed into widespread diseases due to the lifestyle. In arteriosclerosis, the vessels "calcify", become rigid and thus not only promote heart attacks and strokes, but also crack formation in the vessel walls.
Bypass operations, and thus the possibility of induced arteriogenesis, are becoming more and more relevant, especially against this background. However, the induction of arteriogenic processes through external influence is not yet used in clinical practice.













.jpg)




.jpg)


