A Inflammation of the pancreas or Pancreatitis can occur in acute or chronic form. This leads to inflammation of the biliary tract, as can also occur with gallstones. Often, however, abnormal or excessive alcohol consumption is also responsible for inflammation of the pancreas. Since this disease can lead to life-threatening complications, a doctor should be consulted as soon as possible if suspected.
What is pancreatitis?
.jpg)
The pancreas is an organ in the upper abdomen about 15 centimeters long that produces hormones as well as digestive juices and enzymes. If this organ is inflamed by certain factors, it is called pancreatitis. Inflammation of the pancreas, also known as pancreatitis in medical terminology, is a relatively rare disease that either occurs suddenly or can become chronic. In the latter form of this disease, alcohol often plays a role.
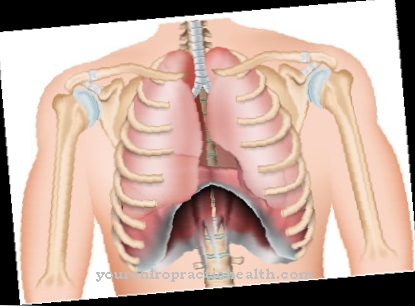
Pancreatitis manifests itself through various symptoms. Most of the patients complain of pain in the upper abdomen and nausea and vomiting are not uncommon side effects of pancreatitis. The abdominal pain can radiate into the back or chest. Patients can often find a hunched back in a lying position, as this eases the pain somewhat.
A soft belly, the so-called "rubber belly", is also typical for pancreatitis. The stomach reacts very sensitively to pressure. If the disease becomes chronic, other symptoms such as weight loss and digestive problems can appear. Jaundice, flatulence and fever are also symptoms that can occur in the context of an inflammation of the pancreas.
causes
Bile duct disorders such as gallstones are often a cause of pancreatitis. But alcohol is also often one of the triggers of this disease. According to statistics, alcohol abuse is the main cause of pancreatitis in men between the ages of 30 and 50, while gallstones are more common in women.
About 1 in 100 people with gallstones will also develop pancreatitis. This happens when a gallstone is placed in front of the exit of the pancreas and blocks it. The digestive juices can no longer escape from the pancreas into the intestines - the result is inflammation of the pancreas.
In addition to alcohol and gallstones, the main triggers of this disease, other factors can also cause pancreatitis. High-fat diets are among these triggers, as are increased blood calcium levels or the use of certain medications. In the rarest of cases, pancreatic cancer is to blame for an inflammation of the pancreas. If the disease is genetic, it is also called hereditary pancreatitis.
Symptoms, ailments & signs
Inflammation of the pancreas can be accompanied by various symptoms. The symptoms that appear depend on whether the patient has acute or chronic pancreatitis. A typical sign of an acute pancreatitis is an abrupt pain in the upper abdomen that is shaped like a belt.
It is not uncommon for the pain to spread to the chest and back, where it lasts for a long time. In addition, the stomach is extremely sensitive and inflates to such an extent that it acts like an elastic rubber belly. If the pancreatitis is caused by gallstone disease, colic-like symptoms are also possible.
In many cases, inflammation of the pancreas is also associated with other symptoms. These are primarily nausea and vomiting. Due to the irritated gastrointestinal tract, feelings of pressure and flatulence also occur in the upper abdomen.
The entire body is affected by the inflamed pancreas. Many patients develop a fever and a general feeling of weakness. The sick person feels tired and weak. Furthermore, the blood pressure often drops.
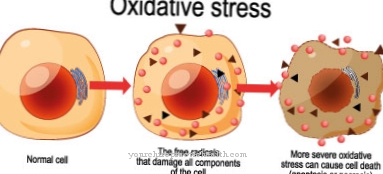
The symptoms of pancreatitis also include increased permeability of the vessel walls. This causes fluid to leak into the adjacent tissue. In extreme cases, this process leads to a breakdown of the circulatory system. Chronic pancreatitis can also lead to fatty stools, weight loss, jaundice and sugar metabolism disorders.
course
In nine out of ten patients, acute pancreatitis runs smoothly and without further complications - it is of course important that it is treated correctly. However, if you repeatedly fall ill with pancreatitis within a short period of time, other diseases such as diabetes can be the unpleasant consequence.
Chronic pancreatitis, in turn, can cause pancreatic cancer. After surviving pancreatitis, patients must pay close attention to their diet: alcohol, coffee and fat in particular are strictly prohibited.
When should you go to the doctor?
Acute pancreatitis requires prompt treatment by the doctor. The family doctor can already carry out the first examinations to narrow down the suspicion. Signals to be taken seriously are sudden abdominal pain that spreads in a circle around the upper abdomen and radiates to the back. If these symptoms persist for no apparent reason, there is sufficient reason to see a doctor. If the inflammation is particularly pronounced, attacks of fever and heavy perspiration are also distinctive features.
The affected people are plagued by nausea and vomiting. In addition, dizziness and falling blood pressure represent a concrete danger to life and limb. In this situation, immediate action is required and valuable time must not pass before help arrives.Therefore, the emergency call is the best choice in the case of severe illness. A rapid rise and the combination of symptoms suggest an acute problem with the pancreas.
In general, there is only a small risk that the disease will go unnoticed for too long due to the frequent intensity of the pain and accompanying symptoms. The chronic form is usually less dominant and develops more slowly, but stresses the body at recurring intervals.
If you consume alcohol and nicotine regularly at the same time, it is also advisable to check your pancreas. In addition to quick help in the event of severe pain, the family doctor usually refers to a specialist to clarify the causes precisely. The gastroenterologist and internist then perform additional examinations to determine the exact location, type and severity of the case.
Doctors & therapists in your area
Treatment & Therapy
The attending physician will first conduct a so-called anamnesis, that is, carefully examine the patient's previous medical history. Several exams like ultrasound, endoscopic exams, and blood tests will find out if this is actually one Pancreatitis. The value of the enzyme lipase is often significantly increased in pancreatitis - an analysis of the blood will quickly determine this.
Acute pancreatitis usually has to be treated in hospital. This therapy usually takes place in the intensive care unit, but conservatively - that is, without surgery. The affected patient is usually not allowed to eat anything until the pain has completely disappeared. During this time, fluids and nutrients are supplied to the body via infusions. This is followed by a slow diet. If gallstones are the cause of the pancreatitis, they are usually removed as part of an endoscopy.
Outlook & forecast
The prognosis of pancreatitis depends primarily on whether it is acute or chronic pancreatitis.
Acute pancreatitis usually heals without long-term damage, although the disease is often very difficult. However, in the course of an acute pancreatitis, complications can also arise that can even be fatal. This is the case, among other things, when the pancreas is almost completely dissolved by the digestive juices.
In a few cases, sepsis (blood poisoning) can occur, which also worsens the short-term prognosis. Other complications, some of which are fatal, include circulatory shock, bleeding in the pancreas and multiple organ failure. After overcoming acute pancreatitis and its complications, there is usually complete healing.
The long-term prognosis for chronic pancreatitis is unfortunately not so good. It doesn't necessarily lead to death. However, chronic complaints can arise. With chronic pancreatitis, inflammatory processes are constantly taking place in the pancreas. This leads to irreversible remodeling processes in the pancreas, which can lead to so-called pseudocysts.
Pseudocysts are chambers filled with fluid. They often become inflamed and sometimes bleed in. Furthermore, calcifications develop in the context of chronic pancreatitis. So-called pancreatic stones often form, which in turn disrupt the outflow of digestive juices. Pancreatic cancer can also develop as a long-term consequence of chronic pancreatitis.
Aftercare
Inflammation of the pancreas (pancreatitis) is a serious disease that should definitely be in the hands of doctors. Consistent follow-up care, in which the patient is also involved, is important after the treatment. Patient cooperation is critical as a variety of causes of pancreatitis are linked to patient behavior.
A classic example of this is alcohol, the frequent consumption of which is considered a typical trigger for inflammation of the pancreas (pancreatitis). If this is the case with the respective patient, abstaining from alcohol in the follow-up care is an essential factor so that the disease does not flare up again. The pancreas and its functions must be consistently spared here. Your family doctor or the treating internist will give you precise rules of conduct.
Pancreatitis requires a conscious diet in follow-up care. The patient can support regeneration by avoiding food that is difficult to digest and opting for a balanced diet. Foods that cause gas such as legumes, fat and cold foods should be avoided.
In addition, there is the aforementioned abstinence from alcohol, which must be followed consistently. Nicotine is also a factor that can have a negative effect on regeneration and is better given up in the sense of a change in lifestyle to a healthy level. Increased blood lipid levels promote inflammation of the pancreas. They can be reduced in the long term through exercise and a change in diet. Regular checks are important.
You can do that yourself
If you don't want to go to a specialist directly, you will find a good alternative in homeopathy. In the early stages, inflammation of the pancreas can be treated well with Phosphorus C5 together with Iodum C5. Take three globules alternately three times until the condition has improved satisfactorily. However, in the case of pancreatitis, it is advisable to see a doctor despite the range of homeopathic preparations and self-help aids.
The most important rule is: Do not drink alcohol. It must not be consumed in pralines or as a flavor in sauces, etc. Likewise, those affected have to do without nicotine. From a health perspective, coffee consumption must at least be reduced. The diet should be extremely high in carbohydrates.
However, overly large portions of lettuce, whole grain products, and fruit and vegetables should be avoided, as this will put too much strain on the digestive system. It is better to eat several small meals throughout the day. These also guarantee an energy supply that is well distributed throughout the day.
Taking a pancreatic powder that can be bought in pharmacies as granules or in capsule form normalizes the frequency of bowel movements and the quality of the stool.
In addition, the fluid intake should be at least 2.5 liters per day. Still water should be fortified with electrolytes. Enrichment is important to prevent the consequences of electrolyte deficiency from the start.

.jpg)
.jpg)

.jpg)





.jpg)



.jpg)










.jpg)
