They are painful and bothersome: Blisters on the feet can turn a hike or a party night into pure agony. However, if you know the causes, you can avoid the formation of blisters on your feet.
What are blisters on the feet?

© mRGB - stock.adobe.com
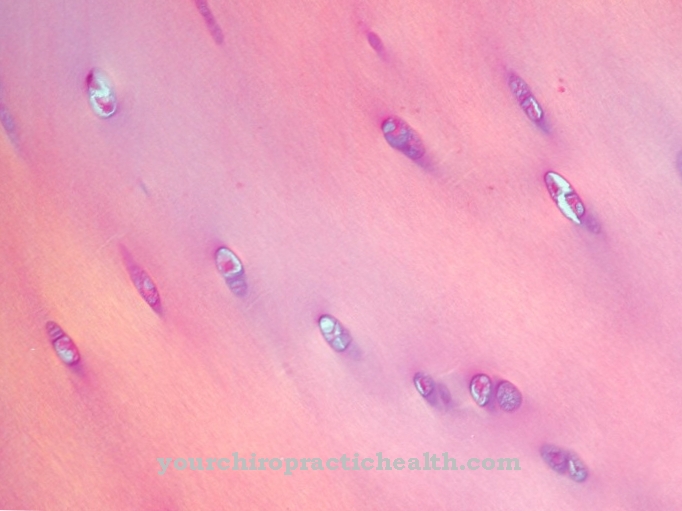
Blisters on the feet are small bumps in the skin that are filled with fluid. Depending on the thickness, blood flow and moisture level of the affected skin area, they can appear light or be very red.
Blisters on the feet tend to occur in places that are exposed to strong friction and are inadequately protected by a natural horny layer. The heels, toes or balls of the feet are often affected: The layers of skin separate from each other, creating cavities between them that fill with tissue water.
The blood bladder is a special form, a superficial bruise caused by impact injuries. Since the nerve cells of the dermis reach into the epidermis, blisters on the feet can be extremely painful.
causes
The main cause of blisters on the feet is shoes that are too tight or poorly fitting. Poor processing of the material can also cause chafing. The formation of blisters on the feet is accelerated by the warm and humid climate in the shoe, which swells the skin and makes it soft and sensitive.
In some cases, too thorough a pedicure also helps to cause blisters to form on the feet: If you file the callus in the heel area too hard, you lose natural protection against blisters on the feet.
In individual cases, however, it can also be a too thick callus that leads to the formation of blisters on the feet: If the horny layer becomes brittle, it lifts off the dermis under stress and a blister forms.
Symptoms, ailments & signs
Blisters on the feet usually appear in three different forms. A distinction can be made between the bladder filled with water, the bladder filled with blood and the open bladder. If blisters develop, this can be perceived at an early stage based on the typical pressure or friction pain that occurs.
The visual inspection in the early stages usually shows a reddened area of skin. To prevent the blister from spreading, the pressure trigger - usually a shoe that is too tight or a crease in the stocking - should be removed. In the advanced stages, the bladder usually first fills with water.
It then shows up as a clearly visible, soft bulge. The pressure and rubbing pain is now increasing and is often perceived as unbearable. The affected person now usually tries to prevent pressure on the bladder with a gentle posture while walking. If deeper layers are affected, blood can now also mix into the bladder fluid so that the bladder appears to be filled with blood. These blisters are no more painful than water-filled blisters.
If friction and pressure are not avoided, the bladder will continue to fill with fluid until the thin skin on its surface bursts and water and blood drain away. The underlying tissue is now open like a wound. The wound pain is felt to be very burning.
Diagnosis & course
Ideally, the diagnosis of blisters on the feet is made very early, namely when a painful reddening of the foot indicates that a blister is developing. Prompt and consistent treatment can sometimes prevent the worst. Anyone who ignores a painful, burning sensation on the foot for too long and waits until the blisters on the feet are fully formed can only wait for the healing process.
This lasts for a few days and begins with the blisters on the feet bursting and the liquid leaking out. The dead epidermis dries up and comes off. A wound will become visible underneath before new skin forms. The healing process is usually straightforward, but diabetics should consult a doctor as a precaution if they have blisters on their feet.
Complications
Blisters on the feet usually lead to pain and reddening of the skin in the affected area. If the outcome is unfavorable, further complications can arise. This can cause pus to develop from the water blisters, increasing the risk of infection and the formation of larger cysts.
If the above-mentioned pus blisters are treated insufficiently or improperly, fistulas and abscesses can develop. If the bubbles break inward, organ abscesses and severe bacterial infections can also occur, and in rare cases life-threatening blood poisoning. In addition, blisters on the feet often lead to malpositions, which do not always go away completely after the symptoms have subsided.
The misalignments can also cause further blisters and skin injuries. In addition, improper treatment can scar the tissue, often accompanied by sensory disturbances and phantom pain. In addition, unhygienic handling of the blisters leads to complications, since pathogens can penetrate the abscess.
Further complications: bleeding after opening the bladder, pain when moving and the formation of fistulas and scar tissue. Most complications can be reliably avoided by early and professional treatment by the family doctor.
When should you go to the doctor?
If you have blisters on your feet, you don't need to see a doctor in most cases. If the bladder is properly cared for, it will recede on its own after a while and will no longer require any follow-up care.
However, there are a few situations that may require a visit to the doctor. If the bladder turns into an open wound on the foot, a doctor should be visited, especially if it is unclear whether a tetanus vaccination is still active. The family doctor is sufficient as a contact person.
Even if a blister turns into inflammation (often due to incorrect care of the bladder or continued increased stress on the broken skin), medical intervention should be taken. Finally, inflammation between the layers of skin in the foot area can become severe. The hygiene and the supply options, especially on the soles of the feet and between the toes, are worse than elsewhere on the skin. An inflamed wound therefore needs the attention of a dermatologist or general practitioner.
A doctor should also be consulted if the bladder does not show any negative development, but also no longer regresses. Most of the time, the bladder on the foot only needs to be properly supplied so that it can regress.
Doctors & therapists in your area
Treatment & Therapy
The treatment of blisters on the feet should begin as soon as the first reddening appears: a packet of blister plasters belongs in every hiking backpack. A modern blister plaster forms a protective cushion over the endangered area and relieves the irritated skin. It is best to change socks as well to reduce skin moisture.
Hikers should also make sure that the foot is free from grains of sand. If the blisters on the feet are already fully developed, they should be opened to relieve pressure. All you need is a needle and a disinfectant. If the tissue fluid has drained from the blisters on the feet, they should be carefully sealed with blister plasters to prevent infections.
If the hike is to be continued afterwards, the plaster must be applied without wrinkles, otherwise new pressure points will form, which will lead to further blisters on the feet. If blisters on the feet are several days old, they become dry and cracked and can be treated with a little zinc ointment.
Outlook & forecast
With blisters on their feet, those affected have very good prospects of recovery. Depending on the size, the blisters can be opened by yourself or with medical assistance. It is important that they are opened sterile and that the open wound is not contaminated. After the bladder opens, it will heal in the coming days. The blister should normally be completely and permanently healed within a week.
If the bladder is not opened, complete healing will also occur. In most cases, the period until the symptoms are free is within the next ten days. In exceptional cases, the organism needs two weeks. The fluid in the bladder is carried away by the body itself and it slowly dries out.
When the bladder bursts, you are at greatest risk of infection. If it comes to contamination, pus can develop due to an inflammatory process. The inflammation should be treated by a doctor so as not to cause further complications. The affected area will usually heal within the next one to two weeks.
If the blisters are caused by wearing tight or unhealthy shoes, the symptoms will return. To avoid the formation of new blisters, shoes should be changed. Alternatively, you can protect your feet by wearing hosiery.
prevention
The best way to prevent blisters on your feet is to choose high quality shoes and break them in well before a long hike. Even on short walks, redness shows which areas could be endangered by blisters on the feet. High-quality cotton socks protect the foot from moisture, while coarse wool socks can quickly lead to blisters on the feet. If you want to avoid blisters on your feet, you should use blister plasters as a preventive measure.
Aftercare
Blisters on the feet don't need follow-up care if they're only superficial. A few days of rest and shoes that don't rub and everything will heal well. But it looks different when several layers of skin are affected by the blister. It can take up to ten days for the bladder to heal completely.
Follow-up care must consist of avoiding further blistering in the same area and protecting the new skin with pads. Follow-up care and precautionary measures before further bubbles are congruent here. Also, blisters on the feet are a dangerous thing to do in diabetic neuropathy.
Blisters on the feet of diabetics not only require prompt and adequate treatment, but also require expert follow-up care. Any untreated injury to a foot that is affected by diabetic neuropathy or otherwise caused circulatory disorders can end in amputation or even fatal. Therefore, aftercare is of particular importance here.
Blisters on the feet are usually harmless in nature. Blisters require follow-up care whenever they heal poorly, become infected, or occur in a diabetic. Burn blisters or blisters that occur after frostbite also require treatment and aftercare on the feet. Such blisters are unlikely to occur on the feet.
You can do that yourself
Under no circumstances should small bubbles be opened. The roof of the bladder consists of intact skin and offers the best protection against infection. A padded plaster provides protection and relieves pressure.
Larger superficial bubbles that are under tension can be punctured. To do this, the needle must be thoroughly disinfected with alcohol. Otherwise the bladder could become inflamed. Then the liquid has to drain off and the skin to dry out. Finally, cover with a plaster that extends over the bladder. The opened bladder can be disinfected beforehand to be on the safe side. Because air helps the healing process, the patch can be removed for the night.
It is important that the skin over a blister is never cut off, as this can lead to inflammation. Some doctors also recommend checking your tetanus protection and possibly having it refreshed.
In homeopathy, a homeopathic mixture (porridge) of Ferrum phosphoricum No. 3 20 and sodium chloratum No. 8 30 is recommended, which accelerates the healing process.
Others prefer Cantharis as a single dose in a high potency to be prescribed by a doctor. Cantharis is freely available in the D12 potency. It should only be taken until the bladder has healed. Then stop immediately. A foot bath in emperor soda (no other baking soda) also helps. Afterwards rub the feet with olive oil.
Diabetics and those who already suffer from a diabetic foot should, as a precaution, consult a doctor directly, otherwise complications can arise.


.jpg)





.jpg)


.jpg)






.jpg)
