Bladder dysfunction is a collective term for all functional disorders of the urinary bladder. This includes all bladder emptying and urinary storage disorders.
What is bladder dysfunction?

© bilderzwerg - stock.adobe.com
The diagnosis of bladder dysfunction is made when the bladder function is disturbed. However, bladder dysfunction is not an independent disease, but rather a collective term for all urinary storage and urination disorders. In the case of urinary storage disorder, the bladder's reservoir function is impaired.
Intentional urination is not possible. In the Voiding disorder it is very difficult to empty the bladder. Functional, mechanical, neurological, and psychogenic factors can be the cause of both forms of bladder dysfunction.
causes
Mechanical causes are mostly responsible for a urination disorder. A mechanical closure is caused by a flow obstruction. The part of the lower urinary tract that is in front of the occlusion increases pressure. Possible mechanical causes of bladder dysfunction are urethral strictures, a urethral valve, bladder stones, or a narrowing of the bladder neck.
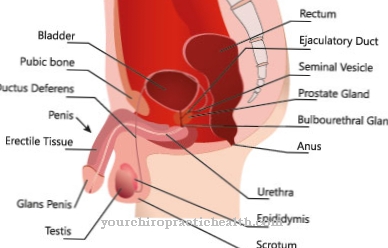
A narrowing of the urethral orifice and a spherical widening of the ureter in the bladder, a so-called ureterocele, can also impair bladder function. In men, a bladder emptying disorder can also be caused by a benign prostate enlargement or by a prostate carcinoma.
Another cause is a pronounced narrowing of the foreskin (buttonhole phimosis). When the nerve supply to the urinary bladder is disturbed, a neurogenic bladder develops. This neurogenic disorder is usually caused by damage to the spinal cord. More rarely, the cause lies in the presacral plexus.
A neurogenic bladder can also develop as part of a Fowler-Christmas-Chapple syndrome. The neurogenic voiding disorder is often also based on multiple sclerosis. Three quarters of all multiple sclerosis patients develop bladder dysfunction in the course of the disease. If the duration of the illness is over ten years, almost 100 percent of the patients have bladder dysfunction. Multiple sclerosis can also be the cause of urinary storage disorders.
Bladder dysfunction in the form of a urinary storage disorder primarily affects older women. Risk factors are cystitis, obesity and diabetes mellitus. Stress incontinence often occurs in women who have given birth naturally to multiple children. Urinary storage disorders can also occur in children and adolescents.
If there is involuntary wetting in children with no apparent physical cause, this is known as enuresis. Bladder dysfunction can also be congenital. The most common causes here are malformations of the urinary bladder. An example of such a malformation is the split bladder. Here the urinary bladder is exposed to the outside.
Symptoms, ailments & signs
If there is a urinary storage disorder, the urine cannot be stored in the urinary bladder without loss. The result is urinary incontinence. There are different forms of urinary incontinence. The most common form is urge incontinence. This is characterized by a sudden, strong need to urinate. This urge is so strong that the toilet cannot be reached in time.
In stress incontinence, the loss of urine is triggered by increased internal pressure in the abdomen. The internal abdominal pressure increases, for example, through strain, pressing, lifting, carrying, laughing, sneezing or coughing. Stress incontinence is also known as stress incontinence. There is also a hybrid of urge and stress incontinence. This is called mixed incontinence.
The overflow incontinence is more a consequence of the urination disorder. If urine remains in the bladder due to drainage problems, an overflow bladder is created. The pressure in the bladder increases until it exceeds the pressure in the urinary system. This creates a constant dripping of urine.
The bladder emptying disorders usually show up through difficult urination (dysuria). This dysuria often occurs in combination with what is known as pollakiuria. With pollakiuria, the affected patients urinate more, but they only excrete smaller amounts of urine. Despite frequent urination, the total amount of urine does not increase.
Diagnosis & course
If bladder dysfunction is suspected, a detailed medical history and clinical examination are carried out. The doctor scans the abdomen. In women, the pelvic floor muscles should also be assessed. In men, a rectal exam is done to assess the prostate. In addition to this clinical examination, imaging procedures such as sonography can provide further information.
These procedures can reveal many causes of voiding disorder. With bladder manometry, a urodynamic examination, the emptying process can be functionally assessed. An assessment of the bladder function is also possible with uroflowmetry. The urine flow is measured. With cystometry, on the other hand, the bladder pressure is assessed during the emptying and storage phase.
To do this, a catheter is inserted into the urinary bladder. Urinary tract infections should be ruled out as a possible cause with urine and laboratory tests. If the examinations do not provide clear results, a cystoscopy can also be performed. Here a mini-endoscope is inserted into the bladder through the urinary tract.
The attending physician can thus gain an insight into the urinary tract and the urinary bladder. Ultrasound, computed tomography, or magnetic resonance imaging are other ways to visualize the bladder and the urinary tract.
Complications
Since bladder dysfunction is a collective term for various functional disorders in the urinary bladder, possible complications depend on the exact cause. If an underlying disease is responsible for the voiding disorder of the bladder, treating it is the priority. With an effective therapy, the complications of bladder emptying and urinary storage disorders can largely be prevented.
Urinary retention (ischuria) is the most feared complication of bladder dysfunction. For various reasons, it can lead to an inability to empty the bladder. These include: drainage congestion in the bladder or urethra, inflammation of the prostate or urinary tract, bladder stones, benign prostate enlargement (benign prostatic hyperplasia) and neurogenic voiding disorders.
Depending on the symptoms that occur, doctors differentiate between a painful, acute urinary retention and a symptom-free, chronic form. Chronic urinary retention often results in overflow incontinence. Due to the risk of rupture of the bladder, acute urinary retention is an emergency.
If the ischuria persists for a long time, the urine backs up into the ureters and kidneys. This damages the kidney parenchyma with the possible consequence of a shrunken kidney.
Other complications of bladder dysfunction include:
- Sepsis,
- Inflammation of the kidney pelvis (pyelonephritis)
- Urine poisoning (uremia),
- chronic renal failure,
- recurrent urinary tract infections.
When should you go to the doctor?
Not every bladder dysfunction requires treatment. A harmless cystitis can also be cured with the good old home remedies such as warmth and bladder tea. It doesn't always have to be antibiotics. But it should improve after a few days. If this is not the case and there is also a fever or recurring urinary tract infections, a doctor, preferably a urologist, should be consulted to clarify the cause. If a bacterial infection is behind the bladder problems, treatment with antibiotics makes sense, for a fungal infection with antimyotics.
In addition to urinary tract infections, bladder or kidney stones or bladder tumors can also cause bladder dysfunction. These are anything but harmless and should be examined by a doctor immediately to avoid complications. Constrictions of the urethra and urinary retention are also a case for the urologist; incontinence usually requires medical help, sometimes psychological support. In principle, it is not wrong to consult a doctor first if you have bladder problems.
Doctors & therapists in your area
Treatment & Therapy
The therapy for bladder dysfunction always depends on the cause. In the case of mechanical problems with voiding the bladder, the obstacle causing the occlusion must be removed. Neurogenic voiding disorders are usually treated with medication.
Treatment with sacral neurostimulation or sacral neuromodulation is also possible. A bladder pacemaker is implanted, which restores the control function of the bladder by emitting weak electrical impulses.
Outlook & forecast
The prognosis for bladder dysfunction depends on the exact type of bladder dysfunction. There are cases in which the full or partial return of bladder control and function can be expected and cases in which this is not to be expected.
In the case of mechanically caused bladder dysfunction, in most cases a way to restore the bladder function can be found surgically. Mostly the fault lies in the urethra or the bladder sphincter, which allows a good prognosis. Urinary retention due to an overstretched bladder can be remedied by temporarily inserting the catheter to drain the urine.
Urinary stones and the like can usually be treated without any problems. Inflammation-related bladder dysfunction will usually go away as the infection heals. In cases where the bladder function is disturbed under certain conditions (pressure, stress, etc.), the prognosis depends on the ability to treat. Medication can often help.
In cases in which the bladder function is no longer guaranteed due to nerve damage, no improvement through medication can be expected. Bladder pacemakers can help, but here too there is no guarantee of success.
Accordingly, there are those affected by bladder dysfunction who will depend on a catheter for the rest of their lives. This is especially true in relation to multiple sclerosis.
prevention
Most voiding disorders are very difficult to prevent. Urinary storage disorders are often the result of weak pelvic floor muscles. Targeted pelvic floor training can strengthen the pelvic floor muscles and thus prevent incontinence.
Aftercare
The term "bladder dysfunction" includes a number of functional disorders. The extent to which follow-up care is necessary depends on the underlying disease. There are cases in which follow-up treatments are not necessary because there are no longer any complaints. This is the case with mechanical dysfunction, among other things.
A surgical procedure here quickly subsides the symptoms. For other people, however, aftercare becomes a lifelong issue. A large proportion of multiple sclerosis patients depend on a catheter. Like all other sick people, you should also observe daily intimate hygiene.
Certain teas also promise relief from the signs. Cold seats are generally to be avoided. Sometimes it also helps if people with bladder dysfunction drink plenty of water and do sports. The symptoms of kidney stones can be reduced in this way. The situation is different when psychological causes cause the dysfunction.
Here, regular treatment proves to be quite time-consuming. A doctor orders psychotherapy to put an end to harmful lifestyle habits. Experience has shown that stress and pressure occur again and again in everyday life, which is why the complaints can arise again if you are upset. Mental and many other protracted causes are often combated with medication.
You can do that yourself
In the case of bladder dysfunction, the effective measures always depend on the cause. For example, urinary retention due to kidney stones can be relieved by drinking plenty of fluids and exercising, while large amounts of water should be avoided in the case of bladder emptying disorders following prostatic hyperplasia.
In general, increased intimate hygiene should be observed during the illness. Those affected can also help the inflammation heal quickly by avoiding cold seats and wearing warm functional underwear. Various care products from the drugstore also help to strengthen the bladder function. A proven natural remedy is horsetail.
The plant can be taken as a tea or in the form of a steam bath and has anti-inflammatory and pain-relieving properties. Couch tea has a similar effect. Herbal teas as well as horseradish, corn tea and calcium-containing foods are also helpful for urinary tract infections or kidney grits. In conjunction with diuretic tea and rest, this usually relieves the symptoms.
Regardless of the tips mentioned, the cause of the bladder dysfunction needs to be determined and, ideally, treated medically. Effective treatment steps can then be initiated together with the doctor.



.jpg)




















