The Blood-eye barrier consists of the blood-retina and the blood-aqueous humor barrier and corresponds to a physiological barrier to ward off pathogens and maintain biochemically different milieus. Disturbances of the blood-retinal barrier cause fluid to accumulate in the area of the retina, which can lead to retinal detachment. Most commonly, diabetes mellitus causes blood-eye barrier disorders.
What is the blood-eye barrier?

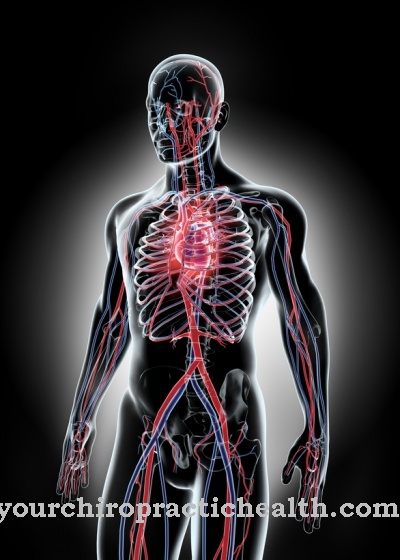
The human body has different biochemical compositions in different places. Physiological barriers maintain these biochemical milieu differences in order to ensure optimal functioning of individual body sections.
One of the most well-known barriers to the separation of different milieus is the blood-brain barrier. The blood-eye-cupboard fulfills a similar function as the blood-brain-barrier. This is a physiological barrier within the eye that separates the uveal blood supply area from the retina.
Furthermore, the blood-eye barrier is responsible for the separation of the anterior chamber and the vitreous body. These two functions are known as the blood-retinal barrier and the blood-aqueous humor barrier. The blood-retina barrier corresponds to the barrier between the retina and the vessels supplying the retina. This barrier is divided into an inner and an outer barrier and has selective permeability. In some literature, the blood-retinal barrier is also referred to as Blood-vitreous barrier viewed.
Function & task
The blood-eye barrier fulfills protective functions. In addition, it maintains the biochemically different composition of the individual eye sections. The blood-aqueous humor barrier ensures, for example, that aqueous humor, vitreous humor and blood plasma do not mix.
The blood-retina barrier, in turn, separates the retina from the plasma. The blood supply to the retina is done by two different blood vessel systems in all mammals. The retinal blood vessels are fed by the central artery and take over the blood supply to the inner retinal layers including their granular layer.
The outer retinal layers and their granular layer as well as sensory cells instead feed on the choroid via diffusion. The outer rods and cones of this retinal layer maintain close contact with the pigment epithelium, the cells of which are connected to one another via tight junctions. Tight junctions are belt-like seams around the entire cell circumference, which form a diffusion barrier in the form of an epithelial cell cluster. This type of barrier is also called a paracellular barrier and closes the intercellular space to protect the interior.
The blood supply to the retina (retina) takes place via the ocular branches of the arteria ophthalmica, via the arteria centralis retinae and the arteriae ciliares posteriores breves. Branches of the central retinal artery run into the strati neurofibrarum et ganglionicum and from there supply the inner parts of the neural retina. The blood supply to the outer photoreceptor layer and the retinal pigment epithelium, on the other hand, comes from the vessels of the choroid of the arteriae ciliares posteriores breves.
In the case of the blood-retinal barrier, the anatomist distinguishes between an inner and an outer barrier. In this distinction, the terms inside and outside refer to the capillaries. The inner blood-retina-barrier is created by tight junctions of the endothelial cells. The outer blood Reina barrier is formed with closely connected epithelial cells in the retinal pigment epithelium.
Both the blood-retinal barrier of the retinal vascular system and that of the choroidal vasculature keep pathogens and toxins from the bloodstream from penetrating the intercellular spaces of the retinal layers. The barriers are selectively permeable. In this way, they keep molecules from penetrating depending on specific properties such as size. Thus, the barriers do not prevent all molecules from passing through.
You can find your medication here
➔ Medicines for visual disturbances and eye complaintsIllnesses & ailments
Disturbances or pathological changes in the blood-retinal barrier always indicate pathological processes within the eye. In addition to macular edema, these pathological processes can also be triggered by retinal hemorrhages and other retinal diseases (retinopathies).
Macular edema is a build-up of extracellular fluid in the yellow spot region. This change is reversible and manifests itself as a blurring of the field of vision, especially in the zone of sharpest vision.
Retinal bleeding, on the other hand, is caused by broken blood vessels. This phenomenon can lead to severe visual disturbances. If edema and retinal hemorrhage are present, the suspicion of a causal blood-retinal barrier disorder is particularly likely.
Isolated disorders of the blood-eye barrier occur in the context of various retinal diseases. A so-called integrity disorder of the inner blood-retinal barrier can occur, for example, in diabetic retinopathy. This is a possible complication of diabetes mellitus. Diabetics often suffer from high blood pressure, which can pathologically change the vessels of the retina in the long term. The changes in the retinal vessels are further promoted by increased or poorly controlled blood sugar. In the course of the process, glycated and otherwise chemically modified macromolecules are deposited in the vessel walls, where they can cause microbleeding in the retina.
In Germany, the blood-retinal barrier disorder as a result of diabetes affects around a third of all diabetics. The risk of diabetic retinopathies for patients with diabetes mellitus is around 90 percent. Diabetic retinopathies can cause blindness over time.
Disorders of the blood-eye barrier do not only occur in the context of diabetes. In the pathomechanism of retinopathia centralis serosa, external blood-retinal barrier disorders are discussed, which correspond to a complete loss of function of the physiological barrier. Retinopathia centralis serosa is an acquired retinal disease with partial retinal detachment, as it seems to arise as a result of functional blood-retinal barrier disorders. Mental and physical stress apparently play a major role in the onset of the disease. The pathogenesis of the disease arises from a disorder of the pigment epithelium. This external blood-retinal barrier disorder causes subretinal fluid retention. The accumulation of fluid leads to the formation of edema, which apparently causes retinal detachment.