Of the Charcot foot represents a rare special form of the diabetic foot. This leads to a softening of the bone, which finally breaks under normal stress.
What is a Charcot foot?

© Aksana - stock.adobe.com
Under a Charcot foot or one Charcot arthropathy Primarily diabetics suffer. 95 percent of all patients are people with diabetes mellitus.
The Charcot foot is a rarely occurring special form of the diabetic foot. One or more bones of the foot become progressively softened in this disease, which ultimately leads to a bone fracture, even though the foot is only exposed to normal loads.
The French neurologist and pathologist Jean-Martin Charcot (1825-1893) gave its name to the Charcot foot. However, the first person to describe the disease was the British physician Herbert William Page in 1881. There are other names for the Charcot foot Neuroarthropathy or Diabetic neuropathic osteo-arthropathy (DNOAP).
causes
How a Charcot foot is created has not yet been determined exactly. A prerequisite for neuroarthropathy is the loss of pain sensitivity in the feet. The disease is usually triggered by a traumatic injury to the skeleton.
There are two theories about the origin of the Charcot foot. These are the neurovascular and neurotraumatic theory. According to the neurovascular theory, nervous malfunctions lead to increased blood flow and more extensive bone resorption.
In the neurotraumatic theory, on the other hand, the view is held that repetitive minor injuries to the joint surfaces are caused by overload because there is a lack of perception of pain. This leads to increasing bone destruction.
Those affected by Charcot's foot are almost always diabetics. In rare cases, however, the condition can also have other causes. These include congenital or acquired neuropathies in which pain perception is impaired, as well as diseases such as syringomyelia, leprosy, syphilis or spina bifida.
Symptoms, ailments & signs
The symptoms of Charcot's foot include several stages. First, there is an accumulation of fluid in the foot. This edema manifests itself as a swelling or red area. However, the patient rarely feels pain, which is due to the damage to the nerves.
If the Charcot foot can be relieved at this stage, the softening of the bones regresses, which takes a period of two to three months. After six to twelve months, the Charcot foot has completely regressed. However, if the normal load on the foot continues, this leads to the continuation of bone loss. Eventually the bone collapses completely.
If the bone fracture appears in the metatarsus, this initially leads to the development of a flat foot. In the further course a rocking foot is formed. If the ankle is affected, there is a risk that the guide will cancel itself out completely. The patient then moves on his or her inner or outer ankle. Pressure points emerge from the misalignments, which then result in blisters or open areas.
As a result, there is a risk of germs entering the body, which can lead to serious infections. In severe cases, this can even endanger the patient's life. In extreme cases, painless impaling of bone fragments through the skin can be observed. Charcot's foot rarely occurs on either foot.
Diagnosis & course
Since the affected people do not even notice the Charcot foot at first, they go to the doctor late. The first thing the medical professional will do is to do a thorough inspection of the foot, which is usually already swollen and inflamed. However, an infection such as a wound rose is usually not present.
Often times the foot is deformed, reddened and heated. It is not uncommon for the doctor to recognize open wounds by the protrusions of the bones. If there are purulent wounds, they can usually be examined painlessly using surgical instruments. There are several examination methods available to the doctor for an exact diagnosis.
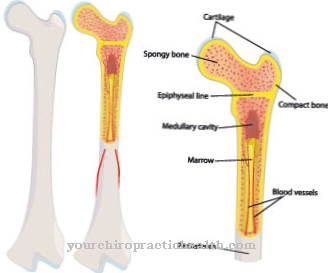
These include x-rays, computed tomography (CT) and magnetic resonance imaging (MRI). White blood cell scintigraphy may also be required to rule out osteomyelitis (inflammation of the bone marrow). Supplementary vascular examinations are carried out if circulatory disorders are suspected.
A Charcot foot can have serious consequences for the patient because he or she does not notice the bone fracture at first. If the patient is no longer able to stand up, complications such as open ulcers threaten. Even after a Charcot's foot has healed successfully, the person affected must undergo medical checks for the rest of their life because there is always the risk of neuroarthropathy again.
Complications
With Charcot's foot, the person affected can suffer a fracture in the foot even with very light loads. This results in extremely severe pain and restricted mobility. As a rule, the breakage does not occur directly. At first the foot only shows swelling and redness and can also be painful.
The pain can in some cases be completely absent due to the damage to the nerves. Furthermore, there is a progressive breakdown of the bone and increasing pain. Likewise, the patient can no longer exert heavy loads on the foot. This has a negative effect on the quality of life.
The treatment is primarily aimed at relieving the strain on the foot. This can lead to significant restrictions in everyday life. In severe cases, a plaster cast is also placed around the foot. Furthermore, a causal treatment must take place that treats the diabetes.
As a rule, there are no particular complications or complaints. Diabetes can be treated relatively well. In the worst case, the Charcot foot has to be amputated if the damage is no longer reversible. Life expectancy itself is not affected by the Charcot foot.
When should you go to the doctor?
If the foot is swollen or reddened, it may be a Charcot foot. If these symptoms have not subsided after a week at the latest, medical advice is required. In the event of restricted mobility or a bone fracture, a doctor must be called in immediately. If no medical treatment is given by then at the latest, painful pressure points, misalignments and infections can occur - medical emergencies that must be treated immediately.
After the hospital stay, depending on the stage of the diabetic foot, protracted physiotherapy therapy is required. Those who suffer mentally from the sudden restriction of movement can also consult a therapist. Mostly diabetics and patients with neuropathies, leprosy, syphilis or diseases of the spinal cord suffer from the Charcot foot.
If you belong to these risk groups, it is best to have the warning signs clarified immediately by the responsible doctor and treated directly on site. In addition to the general practitioner, a diabetologist or specialist can also be consulted for the respective symptom. In the event of a severe course, the emergency doctor must be alerted in any case.
Doctors & therapists in your area
Treatment & Therapy
Acute Charcot's foot is classified as a medical emergency. For treatment, it is therefore necessary to have in-patient care by a specialist who will relieve the pressure completely. In the early edema phase, complete relief lasts three months. In the case of minor burglaries, it may be useful to put on special shoes.
Relieving walking devices such as double-shell orthoses are sometimes used, so that the bone is strengthened again and there is no misalignment. After the acute phase, the foot is given an adapted plaster cast or a rigid plastic bandage. A special orthotic shoe is then worn.
It is also important to normalize the sugar metabolism by treating the diabetes accordingly. In some cases, surgery or even an amputation of the affected foot may be required. The patient receives a lower leg orthosis that can be worn with an orthotic shoe.
Outlook & forecast
In most cases, Charcot's foot can be treated well if the treatment is carried out early and the person concerned changes their circumstances. This is especially necessary for the treatment of diabetes, as the Charcot's foot is triggered by this underlying disease.
The Charcot foot itself receives emergency medical treatment. The patients are dependent on different prostheses or soles to alleviate the symptoms. In severe cases, amputations or other surgical interventions are also necessary. The course here depends heavily on the exact severity of the disease. Therapy should therefore start very early to avoid possible complications.
If the Charcot foot is not treated, the foot can die off completely, whereby other areas of the body are usually affected by inflammation and infections. For those affected, this disease always has severe restrictions on movement and a significantly reduced quality of life.
However, the Charcot foot can be avoided through regular medical examinations. If the person concerned changes their diet and possibly reduces their excess weight, the disease can progress positively.
prevention
Since the Charcot's foot is mostly caused by diabetes mellitus, prevention is not easy. Regular check-ups with a doctor are important.
Aftercare
If the primary treatment by the doctor has been completed, the patient with a Charcot foot should not only adhere to the rules of conduct of the treating diabetologist in order to avoid further complications in the future, but should also actively participate in the follow-up care and prevention of his medical problem. Good blood sugar control is essential in order to avoid further symptoms of the disease.
If the deformation of the foot is very severe, the patient has the option of buying special orthopedic shoes (made to measure). These protect the foot from further damage (costs must be clarified with the health insurance company in advance). The opinion of a specialist in Charcot feet should also be obtained.
As a further follow-up measure, the patient should always take a close look at his or her feet during daily care in order to be able to notice changes early and react if necessary. Particular attention should be paid to pressure points and injuries. Good blood circulation in the feet is achieved if the person concerned does “foot gymnastics” barefoot: stand up, walk around, turn feet and put weight on them.
You should also consider using the services of a professional foot care provider. The money invested here is worthwhile, because the trained specialists not only care for the feet optimally, but also recognize with a trained eye whether and, if so, what changes have occurred to the feet.
You can do that yourself
Acute Charcot's foot is a medical emergency and must be treated by a specialist immediately. Sufferers should go to a hospital immediately.
One of the most important self-help measures is to discover the disease in good time and get treatment. At the beginning of the disease there is usually only a seemingly harmless accumulation of fluid on the foot. The person concerned often does not notice more than redness or swelling.
If the disorder is recognized and treated at this stage, the softening of the bone usually regresses completely over a period of eight to twelve weeks. Members of risk groups should therefore always consult a doctor promptly if they notice edema in the foot area, even if it looks harmless.
Diabetics in particular are among the risk groups. In rare cases, however, a Charcot's foot also forms after infectious diseases such as syphilis. Diabetics help themselves best by fighting the underlying disease. In the case of type 2 diabetes mellitus, this usually means a complete change in lifestyle. It is important to reduce existing excess weight. In addition, a change in eating habits and the integration of sport and regular exercise into the daily routine are almost always necessary.
In the case of an acute illness, all measures to relieve the foot, which the treating doctor has ordered, must be strictly observed. Only in this way is there a chance that the softened bones will recover and the foot will heal again.

.jpg)