Cheyne-Stokes breathing is the name for a pathological form of breathing. There is a regular change in breathing depth and changes in the intervals between breathing.
What is Cheyne-Stokes breathing?

© blueringmedia - stock.adobe.com
Cheyne-Stokes breathing is understood to be a pathological breathing pattern that becomes noticeable through the swelling and decongesting of breathing, which is associated with longer breathing pauses. If breathing periodically flattens out during this process, there is a risk of brief respiratory arrest.
But then deeper breaths start again. Cheyne-Stokes breathing often occurs when the person concerned has insufficient blood flow to the brain. This can be caused, for example, by vascular sclerosis. Other possible triggers are a stroke or poisoning.
The Scottish physician John Cheyne (1777-1836) and the Irish physician William Stokes (1804-1878) gave the Cheyne-Stokes breathing its name. In 1818 John Cheyne succeeded in describing the periodic swelling and swelling of breathing. A short time later, William Stokes followed suit. Cheyne-Stokes breathing is more common in men than in women. The patients are almost always older than 60 years.
causes
The cause of Cheyne-Stokes respiration is a non-linear respiratory center sensitivity to the CO2 partial pressure within the arterial blood. The increase in CO2 partial pressure acts as the strongest breath stimulus. As a result, the breathing rate and the depth of the breaths drop until the higher CO2 content in the blood enables increased breathing.
If the affected person exhales enough CO2, breathing flattens again. Because the sensitivity to CO2 is disproportionately low at low partial pressure and disproportionately high at high partial pressure, this results in the regulator oscillating. In medicine it is discussed whether Cheyne-Stokes breathing can have a negative influence on the course of heart failure.
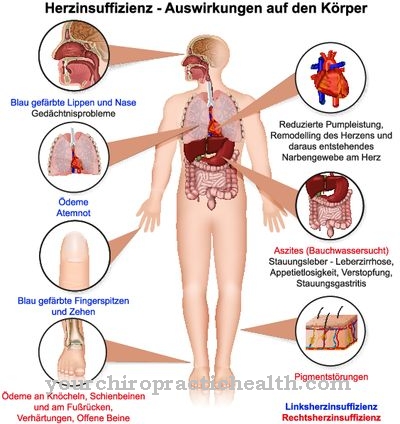
The stronger the cardiac insufficiency, the more intense the periodic and central breathing patterns. The most common triggers for Cheyne-Stokes breathing include an inadequate cerebral blood supply, such as insufficient blood flow in arteriosclerosis, a stroke, or poisoning such as carbon monoxide.
You can find your medication here
➔ Medication for shortness of breath and lung problemsSymptoms, ailments & signs
Cheyne-Stokes breathing is a severe form of breathing disturbance during sleep. It is associated with pronounced forms of heart failure. The prevalence of this pathological form of breathing in heart failure patients is between 30 and 40 percent.
A typical feature of Cheyne-Stokes breathing is the periodically repeating swelling and swelling of breathing. The patient's breaths become more and more flat until a short pause of about ten seconds sets in. Then the breaths become deeper and more strenuous again. In some cases, this process also leads to an additional change in the breathing rate.
Cheyne-Stokes breathing is particularly noticeable at night, in people who suffer from advanced heart failure. Often, however, it also shows up with other damage to the central nervous system such as opioid overdoses, exogenous poisoning or uremia.
Cheyne-Stokes breathing can be the preliminary stage of pre-terminal gasping. Sometimes, however, it also shows up during normal sleep without having any disease value. Cheyne-Stokes breathing often occurs during sleep at altitudes of more than 3000 meters and is called periodic breathing.
Periodic breathing is not classified as a symptom of altitude sickness, but it can cause sleep disorders. In some cases, Cheyne-Stokes breathing wakes the patient up because of shortness of breath.
Diagnosis & course
If Cheyne-Stokes breathing is suspected, a polysomnographic examination in a special sleep laboratory is required. Polysomnography is a diagnostic procedure in which the physiological functions of the patient are measured in a targeted manner while they are sleeping. It represents the most extensive study of its kind.
The examination takes place in an inpatient setting. This gives the doctor the opportunity to create an individual sleep profile for the patient, which makes it easier to diagnose Cheyne-Stokes breathing. As part of the examination, a sleep EEG (brain wave image), EKG (measurement of the heart rhythm), EMG (muscle tension) or EOG (movements of the eyes) can be performed.
Video or audio recordings as well as measuring blood pressure are also possible. If the underlying disease that causes Cheyne-Stokes respiration is successfully treated, the patient's prognosis is usually positive.
Complications
Cheyne-Stokes breathing has serious respiratory complications, most of which occur during sleep. The symptom is also closely related to heart failure. The patient's breathing rate also changes over time, which has negative effects on the health of the body.
The changed breathing can also damage the patient's nervous system, whereby Cheyne-Stokes breathing can also manifest itself in the form of gasping. The person concerned is not directly awakened by the wrong breathing, so that many patients can sleep without discomfort. As the disease progresses, however, the patient suffers from insomnia and wakes up because he suffers from shortness of breath.
Often the shortness of breath is accompanied by a panic attack. Cheyne-Stokes respiration is usually treated causally and is primarily aimed at treating kidney failure or diabetes. Thereafter, the patient has to undergo ventilation therapy to prevent consequential damage. Complications usually only occur if the wrong breathing is not treated or if there are complications due to the underlying disease.
When should you go to the doctor?
If the characteristic swelling and swelling of the breath is noticed, a doctor should be consulted. On the one hand, medical clarification is necessary due to the possible risks of a disturbed breathing pattern. On the other hand, Cheyne-Stokes breathing is often based on a serious condition that needs to be diagnosed and, if necessary, treated. A medical clarification is therefore necessary at the latest when complications arise from the breathing difficulties.
Cheyne-Stokes respiration mainly affects people who suffer from arteriosclerosis or who have suffered a stroke. Carbon monoxide poisoning can also cause the disturbed breathing rate. The disease is also associated with diabetes mellitus, kidney failure, heart failure and a few other diseases.
Anyone who belongs to these risk groups should speak to their family doctor immediately if they experience the symptoms mentioned. Other contacts are the pulmonologist or a sleep laboratory. Parents who notice an unusual breathing pattern in their child are best to speak to the pediatrician. In the event of extreme shortness of breath or signs of insufficient oxygen supply, the emergency services must be alerted.
Doctors & therapists in your area
Treatment & Therapy
Cheyne-Stokes breathing therapy consists of two stages. In stage 1, the underlying disease causing the disease is treated. This can be heart failure, kidney failure, diabetes mellitus (diabetes) or other diseases.
Stage 2 provides for ventilation therapy. Its aim is to transform the pathophysiological breathing pattern into a physiological breathing pattern. AZMV (countercyclically modulated ventilation) or ASV (adaptive servo ventilation) are common ventilation methods. In these procedures, a mask system is placed on the patient. It enables automatic breathing pressure regulation.
It also dampens the oscillation of the regulation in a mechanical way. The breathing fluctuations caused by Cheyne-Stokes breathing are counter-cyclically balanced, while the pathophysiological breathing patterns take a physiological direction.
In the case of some patients, the administration of additional oxygen can also linearize the respiratory response curve and thus dampen the fluctuating respiratory regulation. If the patient suffers from altitude sickness, it is necessary to descend immediately into lower regions until all symptoms improve. In this way he again receives a sufficient supply of oxygen.
Outlook & forecast
As a rule, the further course of Cheyne-Stokes respiration depends to a relatively large extent on the underlying disease. It is therefore not possible to make a general statement about the prognosis for this disease. If the underlying disease can be cured, it usually also combats Cheyne-Stokes breathing.
However, most of the symptoms of the heart or kidneys cannot be completely resolved, so that the symptoms of Cheyne-Stokes breathing are not completely restricted. In the case of diabetes, the disease can usually be suppressed relatively well. Chronic complaints are also limited by special ventilation therapy. A complete healing is not achieved thereby either. In the case of altitude sickness, Cheyne-Stokes breathing can also be released by descending. The complaints usually reappear when the person concerned goes to a great height.
In many cases, the disease can also be alleviated by means of self-help or by not using drugs. Ventilators can also be used in your own home, so that an inpatient stay is not absolutely necessary for the patient. Relaxation exercises can also reduce the symptoms of the disease.
You can find your medication here
➔ Medication for shortness of breath and lung problemsprevention
There are no known preventive measures against Cheyne-Stokes breathing. Regular medical examinations are important.
Aftercare
With Cheyne-Stokes respiration, the follow-up measures are in most cases very limited. In the case of this disease, early detection is very important in order to avoid further complications or complaints. The earlier Cheyne-Stokes respiration is recognized by a doctor, the better the further course of the disease will usually be.
This disease may also lead to a reduced life expectancy. For this reason, the person concerned should consult a doctor as soon as the first symptoms and signs of the disease appear, so that the symptoms do not worsen further. The treatment itself depends on the underlying disease.
If this is treated by a surgical procedure, it is advisable for those affected to rest after the procedure and refrain from physical or stressful activities. It is also important to ensure a healthy lifestyle with a healthy diet. However, in many cases it is also necessary to take medication to relieve symptoms.
It is important to ensure that it is taken regularly with the correct dosage. The further course of Cheyne-Stokes respiration depends heavily on the underlying disease, so that no general course can be given.
You can do that yourself
Cheyne-Stokes breathing can be triggered by a changed breathing rhythm, brain damage or a pathological heart defect. Those affected must therefore be able to initiate various measures for self-help in their everyday lives and instruct their relatives accordingly.
The syndrome mostly occurs at night during sleep phases. Breathing pauses and increased wake-up reactions by the body. A healthy deep sleep is not possible. The fear of total respiratory arrest can affect those affected so strongly that a normal life course no longer seems possible. Patients with Cheyne-Stokes breathing often appear very overtired and exhausted.
It is very important to have a balanced lifestyle and to refrain from alcohol, smoking and drugs of any kind. Stimulants or drugs that induce sleep do not serve to help themselves, but have a physically destructive effect. A balanced diet rich in vitamins is also advisable, especially for patients with heart failure and overweight.
Ventilators for household use are increasingly being used as a sensible form of self-help. Before doing this, however, the syndrome should be carefully examined in a sleep laboratory. Regular therapeutic oxygen administration and regulating medication help the patient to cope better with everyday life. To control breathing and maintain lung capacity, gentle exercise such as yoga and swimming can be supportive. Avoid stress, extreme physical exertion and high-fat food.


.jpg)







.jpg)



.jpg)










.jpg)
