Probably each of us has felt the unpleasant sensations that a bad stomach triggers on our own body. Sudden feeling of pressure and fullness in the epigastric region, nausea, nausea and finally vomiting leading to relief are the signs that indicate an acute gastric mucosal inflammation. An excess of food or incorrectly composed dishes are usually the causes of this evil.
How the stomach works
.jpg)
© Alex - stock.adobe.com
But short-term tea fasting, rusks and the application of heat to the stomach area soon smooth these waves. However, if the described symptoms persist and complications such as diarrhea and fever occur, the doctor must be consulted immediately, as the symptoms may conceal bacterial diseases, serious metabolic disorders or various types of poisoning.
The stomach, a muscular hollow organ, is used to absorb the food that has already been crushed in the mouth and mixed with the fermented saliva. In addition, the gastric mucosal glands secrete the digestive gastric juice, which consists of hydrochloric acid, pepsin and other important ferments. If the vigorous muscle work of the stomach wall has resulted in a good mixing of the food with the gastric juice and the possible pre-digestion inside the stomach, the liquefied chyme is emptied into the duodenum in portions through the porter's muscle at the stomach outlet.
A ferment system alerts the major digestive glands, the liver and the pancreas, and they pour their secretions, bile and pancreas into the duodenum via the chyme. The gastric mucous membrane is normally able to protect itself effectively against self-digestion through the strong production of mucus by the acidic, extremely ferment-active gastric juice. The various physiological digestive processes of the stomach are controlled by the vegetative part of the nervous system, which is in constant interrelation with the cerebral cortex.
The function of the stomach is therefore at the center of all digestive processes, and it is evident that various disturbances can arise in the course of these intricate processes. In contrast to the acute inflammatory gastric disease, there is inflammation of the mucous membranes with a chronic tendency, which harbors a serious health risk. The main danger is that many sick people keep postponing going to the medical examination because of the subliminal but persistent complaints.
Unfortunately, the bearable pain is endured for too long, as it can just be reconciled with daily tasks. When asked by the doctor, patients who have manifested stomach ailments often write: "I've actually had stomach problems for many years!"
Symptoms, ailments & signs
Chronic gastritis or chronic gastric catarrh is a persistent disease of the mucous membrane of the stomach with impaired digestive performance. Chronic gastritis develops slowly over a longer period of time and does not cause any symptoms or discomfort at the beginning. The typical signs are similar to those of acute gastritis.
The patients complain of persistent pressure and a feeling of fullness in the upper abdomen, especially after eating, of reluctance to eat the pain-inducing food, acid eructation, a coated tongue, and sometimes heartburn. The patient's surroundings are struck by his pallor, depressed mood, and a foul odor from his mouth.
He himself is reluctant to work because his performance is reduced and he is never symptom-free. After a long period of illness there is weight loss, in severe cases vomiting, which can even be bloody. These complaints are not of a continuous nature, rather they appear periodically.
The forms of gastritis are divided into three types: Type A gastritis causes a vitamin B12 deficiency, which manifests itself as signs of anemia. As the disease progresses, type gastritis can develop into stomach cancer. In type B gastritis, concomitant diseases such as duodenal ulcers, MALT lymphoma or gastric cancer can occur, each associated with pain, feelings of pressure in the affected area and increasing malaise.
Type C gastritis manifests itself primarily as a growing feeling of illness. This is accompanied by the symptoms of an irritable stomach, i.e. frequent abdominal pain, sensitivity to cold, hot or spicy foods as well as recurring gas and diarrhea. In general, the symptoms of chronic gastritis increase in intensity over the course of months or even years and usually cause secondary diseases of the gastrointestinal tract.
To establish the diagnosis, gastric juice is obtained through a thin stomach tube and its acidity is determined chemically. It can be increased, decreased, but also normal. The X-ray examination of the stomach, which must always be carried out, is primarily used to distinguish it from a gastric ulcer or gastric cancer.
Complications
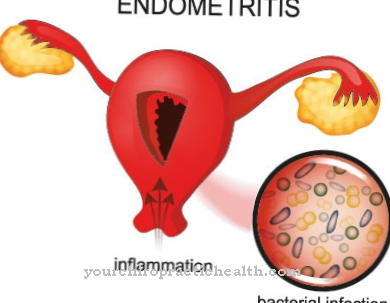
The different types of chronic gastric mucosal inflammation can have different complications. With chronic gastritis type A there is an increased risk of gastric cancer. The increased secretion of gastrin can also lead to the formation of malignant stomach tumors.
The reduced vitamin B12 intake can lead to pernicious anemia, a form of anemia. In type B, a common complication is the development of gastric and duodenal ulcers. This can also lead to Helicobacter pylori gastritis, which changes the lining of the stomach and increases the risk of stomach cancer.
So-called MALT lymphomas, malignant growths in the lymph tissue that can spread to the lungs, salivary glands or thyroid gland, also rarely develop. Chronic Ty-C gastritis also has an increased risk of malignant changes in the abdomen. In addition, chronic inflammation of the gastric mucosa is often associated with bleeding and severe pain.
If left untreated, the surrounding organs can become inflamed, leading to severe infections and organ failure. In the treatment of gastritis, the risks come primarily from the prescribed medication, which can lead to allergies and, due to the combination of different preparations, also to serious side effects.
When should you go to the doctor?
Stomach pain that recurs or that lasts for a long time without an apparent cause should be clarified by a doctor. This is especially true if there are other symptoms such as loss of appetite, nausea, vomiting or constant fatigue. The first point of contact is the family doctor: If, based on the symptoms and the clinical examination, there is a suspicion of chronic gastric mucosal inflammation, he or she will order a gastroscopy to be performed by the internist.
The family doctor should also be consulted if stomach pain could be due to the use of certain medications. In this case, the doctor will, if possible, switch to better tolerated drugs or prescribe tablets to protect the stomach. A doctor's visit is urgently recommended if chronic gastric mucosal inflammation is associated with rapid weight loss. Black stools, vomiting blood, and severe, sudden stomach cramps are also warning signs that require immediate treatment by a doctor or hospital.
If the chronic gastritis is caused by mental overload, a conversation with a psychotherapist can help to process stress and problems better. Even if chronic gastric mucosal inflammation is largely symptom-free, regular check-ups are advisable if the disease is known: In this way, incipient complications such as a stomach ulcer or anemia can be detected and treated in good time. In addition, any inexplicable deterioration in the general condition should immediately result in a doctor's visit.
Doctors & therapists in your area
Treatment & Therapy
The diagnosis of gastritis can only be assumed radiologically, but not made with certainty. Obtaining gastric mucosa and examining it under the microscope as well as examining the gastroscopy directly on the gastric mucosa provides much better information. The chronic inflammatory changes in the gastric mucosa can lead to both growth and flattening.
The dangers of chronic gastritis are that a gastric ulcer (loss of substance in the stomach wall) and, over the years, cancer (increase in substance through abnormal cell proliferation) can develop on the basis of such a permanent irritation of the gastric mucosa with increased cellular restructuring.
What causes lead to chronic inflammation of the stomach lining (gastritis)? Insufficient chewing, eating too hastily, food that is too hot or too cold, damaged teeth, purulent diseases of the nasopharynx and its sinuses. Vitamin deficiency and, above all, chronic abuse of alcohol and nicotine, chronic alcohol consumption, especially on an empty stomach, can contribute to the destruction of the gastric mucosa and the drying up of acid secretions.
The bacterial colonization that this makes possible maintains chronic gastritis. In addition, there are persistent mental states of tension due to professional and family discrepancies; Excessive demands on performance, insufficient recovery phases and poor sleep, especially in combination with the factors listed above, can be observed as the triggering causes of chronic gastritis.
A promising treatment requires patience from the doctor and the patient, a thorough investigation of the causes present in the individual, consistency and insight into the necessities, that is, the potentialist must avoid everything that is harmful to him, especially alcohol and nicotine. He must adhere to the prescribed light diet, carry out heat treatments, have bad teeth and foci of pus removed and must create order in his way of life and work. The acidification of the stomach or the lack of hydrochloric acid require medical control.
Many sick people can be cured by these measures without sick leave, but there are also cases in which strict inpatient treatment in a medical clinic is necessary. The patient must be willing to let his attending physician guide him psychologically and to give up all harmful habits. A change of job may even be necessary.
Outlook & forecast
The course of chronic gastritis depends on its cause and form. Since an inflammation of the gastric mucous membranes is often not noticed for a long time, permanent damage may already have occurred, which can last for a lifetime despite extensive treatment. There is no cure for autoimmune gastritis. However, it does not significantly reduce the quality of life and only progresses slowly with appropriate treatment. Regular endoscopic checks can diagnose and treat any secondary diseases such as stomach cancer at an early stage.
Chronic gastric mucosal inflammation of type B can be cured in 90 percent of cases. If antibiotic therapy is started early, the disease usually clears up within six to eight weeks. Relapses and secondary symptoms are unlikely with this form of gastritis.
Chronic type C gastritis usually heals without any sequelae or recurrence, provided the doctor can determine the chemical cause of the inflammation and eliminate it. If the trigger cannot be determined, symptomatic treatment is possible. The chronic gastritis itself, however, persists and repeatedly causes complaints that require individual treatment.
prevention
In the knowledge of the causal importance of chronic atrophic gastritis for the occurrence of gastric cancer, the demand of medical science will be more and more established that chronic gastric patients should be examined regularly as part of preventive care. This is the only way to recognize malignant degeneration at an early stage and to remove it successfully through a surgical procedure. Sick people with pernicious anemia (a form of anemia (anemia) based on a lack of vitamin B12), who are much more likely to develop gastric cancer than healthy comparators, must also be included in the group of people at risk.
The gastric patient must be open-minded and understanding towards these prophylactic measures, even if swallowing a gastric tube or a gastroscopy is often found unpleasant. Since this proven diagnostic measure, especially for the extraction and examination of cell material from the inside of the stomach, can hardly be dispensed with, it should not go unmentioned that work is being carried out on facilitating methods.
As stated, chronic gastric mucosal inflammation is only a symptom of a general disease that only manifests itself in the stomach. A regular daily routine, a well-proportioned relationship between stress and relaxation, avoiding harmful effects and regular consumption of easily digestible food can protect your stomach from serious damage.
Aftercare
Follow-up care for chronic gastritis depends primarily on the cause of the inflammation that has developed. Type B gastritis caused by the bacterium Helicobacter pylori is by far the most common form of chronic gastric mucosal inflammation and requires success control after therapy has been carried out. The aim here is to ensure that the bacteria have been adequately eliminated by the administration of medication.
This follow-up care can usually be carried out non-invasively with a stool or breath test. If, however, extensive damage to the mucous membrane or a gastric ulcer was already present at the time of diagnosis, a gastroscopy and sampling must be performed again in order to assess the extent of the damage. The patient should decide this individually with his treating doctor.
The autoimmune-related type A gastritis also requires regular monitoring, since the autoimmune reaction can cause degeneration. In order to identify any malignant cells in the stomach as early as possible, an endoscopic control with a gastroscopy should therefore also be carried out. Every patient with chronic gastritis should discuss with their family doctor whether they should make certain dietary changes.
In addition, symptoms such as frequent heartburn, stabbing stomach pains or vomiting blood must be linked to the previous history and clarified in the future. It is advisable to take acid protectants such as omeprazole or the like to protect the stomach when these symptoms occur. However, this should be discussed with the doctor.
You can do that yourself
Measures that can be taken even with chronic gastritis depend on the cause of this inflammatory disease. In the case of proven bacterial infestation, natural substances can also help in addition to antibiotic therapy. The oil from grapefruit seeds acts like a natural antibiotic and kills the germs in the stomach. In addition to conventional treatment, it is also advisable to take healthy intestinal bacteria. These support the entire immune system and in the event of a bacterial attack or antibiosis, the intestine is usually also damaged.
In general, checking your own diet is the first step in self-treatment. Irritant foods and drinks (spicy, hot, fatty, alcoholic) should be avoided, sufficient fluid intake (still mineral waters, unsweetened herbal teas) should be ensured, and several small meals spread throughout the day relieves the stomach.
Thorough chewing also helps the stomach work. A diet rich in vital and minerals strengthens the entire organism.If drugs irritate the gastric mucosa, we recommend a consultation with the attending physician and the exchange of the preparation.
Chronic gastric mucosal inflammation is not infrequently the result of too stressful everyday life. Small breaks - even during working hours - and walks in the fresh air help here. Light endurance sports such as swimming or jogging are also a very good way of achieving physical and mental balance.


.jpg)







.jpg)



.jpg)










.jpg)
