Chymotrypsin B belongs to the digestive enzymes. It is produced by the pancreas and plays an important role in the digestion of proteins.
What is chymotrypsin B?
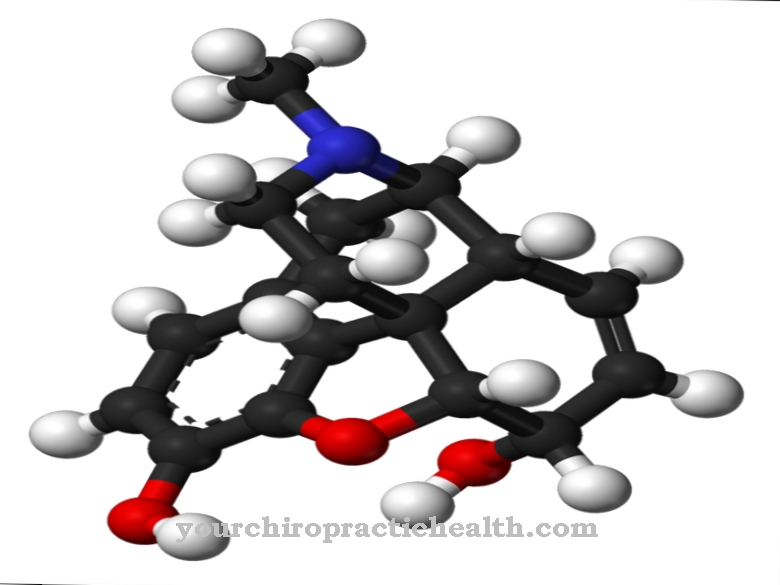
Chymotrypsin B is a digestive enzyme and belongs to the serine proteases. Serine proteases are in turn a subgroup of the peptidases. Peptidases are enzymes that can break down proteins.
Serine proteases are characterized by the fact that they have the amino acid serine in their active center. Other digestive enzymes that belong to the serine proteases are trypsin, elastase and plasmin. Chymotrypsin B is very similar in its chemical composition to trypsin. The effect of the two digestive enzymes is slightly different, however.
Function, effect & tasks
Chymotrypsin is made in the pancreas. So that the pancreas does not digest itself with this enzyme, it is first formed in the form of the inactive chymotrypsinogen. It is activated in the small intestine by the chemically similar digestive enzyme trypsin.
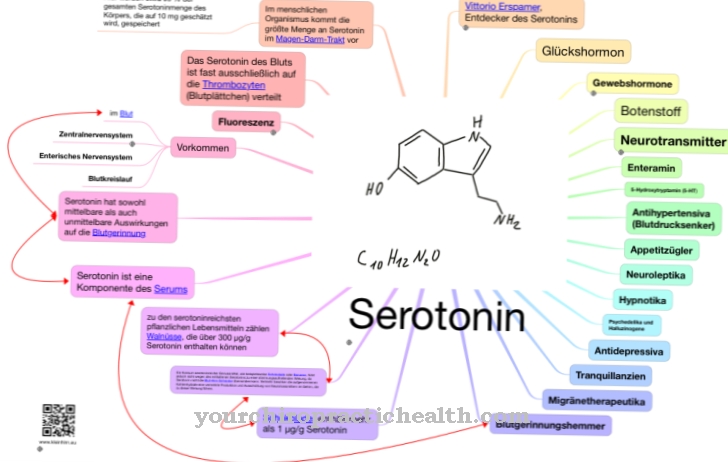
Trypsin is also released into the small intestine in its inactive form. It is activated there by an enterokinase and can then ultimately also activate chymotrypsin B. Chymotrypsin B is released into the small intestine along with many other digestive enzymes in pancreatic secretions. The pancreas produces about one and a half liters of this secretion per day. It is strongly alkaline because it is supposed to neutralize the chyme, which is very acidic after mixing with the gastric juice. The digestive enzymes of the pancreas cannot do their job when the pH is acidic.
The secretion of the pancreatic juice and thus also the secretion of chymotrypsin B is primarily stimulated by the hormones cholecystokinin and secretin. Cholecystokinin and secretin are released from the cells of the small intestine as soon as they come into contact with acidic chyme. The hormones glucagon, somatostatin, peptide YY and the pancreatic polypeptide, on the other hand, inhibit the release of pancreatic secretions including its hormones. Less chymotrypsin B is also secreted under the influence of the sympathetic nervous system.
Chymotrypsin B is excreted in the stool. The values for the digestive enzyme are therefore also measured in the stool. For chymotrypsin in stool, a reference value of> 6 U / g stool applies to adults. The chymotrypsin value provides information on the function of the pancreas. An increased excretion of chymotrypsin has no disease value. A lowered value can indicate a functional weakness of the pancreas.
Education, occurrence, properties & optimal values
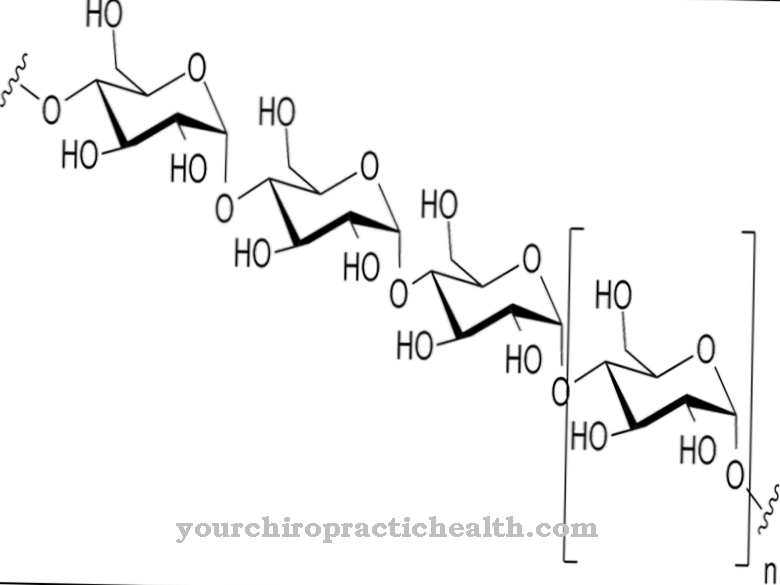
Chymotrypsin B has the task of breaking down proteins in the small intestine. The enzyme works most effectively under basic conditions. The digestive enzyme pepsin already starts to break down proteins in the stomach. Here the proteins are broken down into peptides.
In the small intestine, protein breakdown is then continued by chymotrypsin B, among other things. The already shortened protein chains are broken down into individual amino acids by the digestive enzyme. In this form, the small protein components can be absorbed by the intestinal mucous membrane and reach the liver via the blood. There they are further processed. In contrast to trypsin, chymotrypsin B also has a milk-clotting effect.
Diseases & Disorders
A deficiency in chymotrypsin B is usually associated with a deficiency in all pancreatic enzymes. This deficiency is usually a result of a pancreatic disorder. This is also referred to as exocrine pancreatic insufficiency (EPI).
The disease can have various causes. In children, the most common cause is cystic fibrosis. This is a congenital hereditary disease characterized by thick secretions in various organs. In addition to the lungs, this also includes the pancreas. In adults, the EPI is usually the result of severe inflammation of the pancreas (pancreatitis). Acute pancreatitis with tissue destruction is usually caused by gallstones or infections with viruses. Chronic pancreatitis usually results from alcohol abuse. But other genetic or idiopathic diseases can also cause insufficiency of the pancreas.
As a result, the pancreas can only produce the enzymes or the precursors of the enzymes such as trypsinogen or chymotrypsinogen to a limited extent. If these enzymes are now missing in the digestive tract, the proteins can no longer be broken down and, as a result, can no longer be absorbed by the intestinal mucosa. This digestive disorder is also known as maldigestion. This also puts a strain on the intestinal mucosa.The villi of the intestine atrophy and inflammation develops. Often there is also an incorrect colonization of the intestine with harmful bacteria.
The disease manifests itself through chronic weight loss. Physiological weight gain does not occur in children. Even increased food intake cannot stop weight loss or lead to weight gain. The stool of those affected is rather light. It smells bad and is voluminous. In medical terminology, this is referred to as steatorrhea, a fatty stool. But diarrhea can also occur. If too little vitamin K is absorbed through the intestinal mucosa, this can result in an increased tendency to bleed. The secretin-pancreozymin test should normally be used if pancreatic insufficiency is suspected. However, since this is very complex, the concentration of the enzymes elastase and chymotrypsin in the stool is usually determined using a fluorescein dilaurate test.
In acute pancreatitis, the pancreas self-digest (autodigestion). Chymotrypsin B is also involved here. Blocking the pancreatic duct with gallstones leads to a backlog of pancreatic juices and secretions from the small intestine. The convertase, which activates the trypsinogen, is contained in the secretion of the small intestine. Once activated, trypsin activates the other digestive enzymes as well. The digestive enzymes begin their work within the pancreas and break down fats, carbohydrates and proteins. But these are the fats, carbohydrates and proteins that make up the pancreas. This leads to severe inflammation.

.jpg)