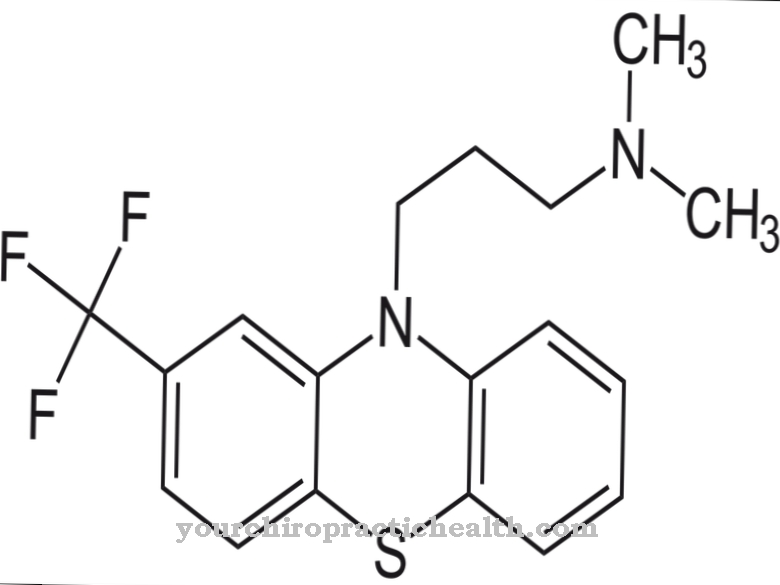
Clozapine is a neuroleptic. It is used to treat schizophrenia and psychosis when other drugs are unsuitable.
What is clozapine?
The prescription antipsychotic clozapine belongs to the group of neuroleptics. The active ingredient is used when other drugs in the treatment of psychoses or schizophrenia either do not show the desired effect or the patient cannot tolerate them. Before using the neuroleptic, a blood count of the sick person must be taken.
Clozapine was developed at the end of the 1950s by the Swiss Wander AG. A screening for the production of new antidepressants was carried out among around 2000 different substances. The active ingredient was patented in 1960, although its antipsychotic effects initially remained undiscovered. In the mid-1960s, further experiments were carried out on people suffering from chronic productive schizophrenia. As part of the studies, the researchers finally noticed the antipsychotic effects of clozapine.
The drug came onto the market in 1972 under the product name Leponex®, which was often prescribed in Europe. In 1975, however, several patients in Finland had agranulocytosis cases with fatal outcome, for which clozapine was responsible. For this reason, several states such as Germany issued special regulations for the use of the drug. The doctor was obliged to inform the manufacturer of the prescription for clozapine, whereupon he received an information package about the agent. He was only allowed to prescribe the antipsychotic after the doctor had given him a written assurance that he would take the data into account. In 1990, the active ingredient was also launched on the US market under the trade name Clozaril®. Several generic drugs were released in the following years.
To date, despite numerous research efforts, clozapine has remained the only drug of its kind that does not cause Parkinson's symptoms in high doses. Since other neuroleptics such as risperidone or quetiapine do not involve a higher risk of agranulocytosis, they are often preferred to clozapine.
Pharmacological effect
Clozapine is one of the atypical neuroleptics. This means that it is bound to the receptors of the messenger substances serotonin and dopamine in the central nervous system, where it blocks the docking points. If there is an excess of dopamine, this is noticeable in a changed mindset and self-perception. In addition, delusions are possible.
By blocking the dopamine receptors, clozapine allows the brain to return to normal. Anxiety disorders and states of agitation are alleviated and concentration and memory improve.
The absorption of clozapine into the blood takes place almost entirely through the gastrointestinal tract. Most of the metabolism takes place within the liver. The active ingredient is excreted in the stool and urine. It takes 8 to 16 hours for the clozapine to leave the body.
Medical application & use
Clozapine is used to treat severe schizophrenia. However, since the neuroleptic has strong side effects, it is only used if other drugs do not improve the symptoms. The same applies to the fight against severe psychoses in the context of Parkinson's disease. Here, too, treatment only takes place after the usual therapy has failed.
In most cases, clozapine is given in tablet form. Sometimes a syringe can also be used. How high the dose of the neuroleptic is determined by the attending physician on a case-by-case basis. As a rule, the patient initially receives a low dose, which is then gradually increased as the therapy progresses. When the treatment comes to an end, it is advisable to slowly reduce the dosage again.
Before clozapine therapy can take place, the patient's blood count must show a normal white blood cell count. This means that the number of leukocytes (white blood cells) and the differential blood count must correspond to normal values.
You can find your medication here
➔ Medicines to calm down and strengthen nervesRisks & side effects
Since treatment with clozapine can lead to leukopenia (lack of white blood cells) or agranulocytosis (lack of granulocytes), it is necessary to subject the patient to regular blood counts during treatment.
The most common side effects of the neuroleptic include palpitations, constipation, drowsiness and excessive salivation. Furthermore, there are visual disturbances, an increase in weight, a drop in blood pressure after getting up, tremors, headaches, tics, problems sitting still, seizures, loss of appetite, nausea, vomiting, high blood pressure, dry mouth, fever, problems with temperature regulation and difficulty urinating possible. In rare cases, there is a risk of hypoglycaemia including metabolic imbalance, severe cardiac muscle inflammation, circulatory collapse, acute pancreatitis or severe liver necrosis, in which the liver tissue dies.
If the patient is hypersensitive to clozapine, the use of the neuroleptic must be avoided. The same applies if the patient had agranulocytosis, blood count disorders or bone marrow damage during previous clozapine therapies.
In addition, the patient must not receive any substances during treatment that could cause blood disorders. Further contraindications are poisoning-related psychoses, untreated epilepsies, clouding of consciousness, pronounced disorders of brain performance, jaundice, diseases of the liver, heart or kidney diseases and intestinal paralysis.
Treatment of pregnant and breastfeeding women with clozapine is prohibited. There is a risk that the children will be harmed by withdrawal symptoms or movement disorders.
Interactions with other drugs can also occur. For example, the effects of clozapine are enhanced by taking erythromycin and cimetidine. In addition, nicotine and caffeine affect the effects of the neuroleptic, so the patient should not suddenly change their consumption during treatment.