Dehydrogenases are enzymes that are involved in oxidation processes. They occur in different variants in the human body and, for example, catalyze the breakdown of alcohol in the liver.
What are dehydrogenases?
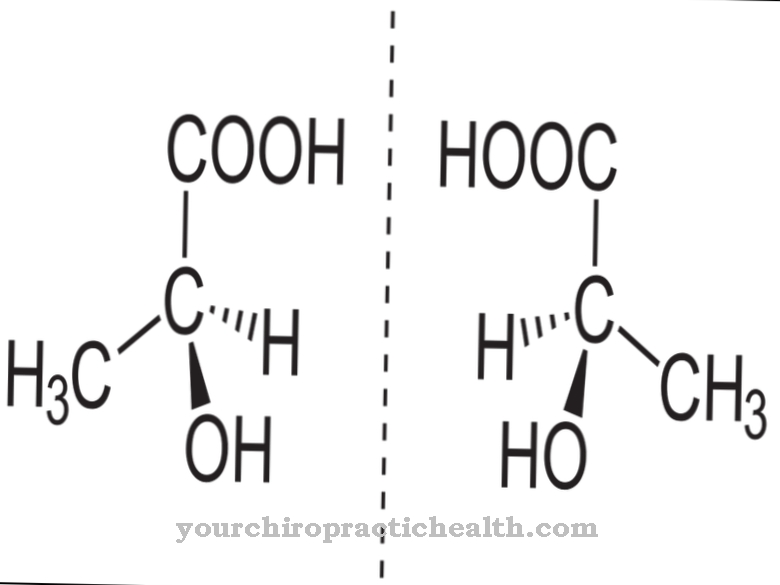
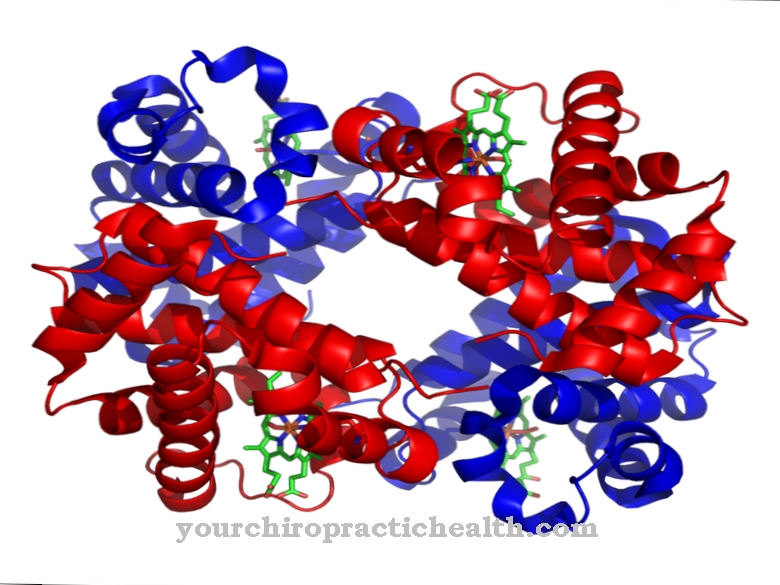
Dehydrogenases are specialized enzymes. The biocatalysts accelerate the natural oxidation of substrates. A substance that oxidizes loses electrons. In biological reactions, dehydrogenases split off hydrogen anions from a substrate. Anions are negatively charged particles.
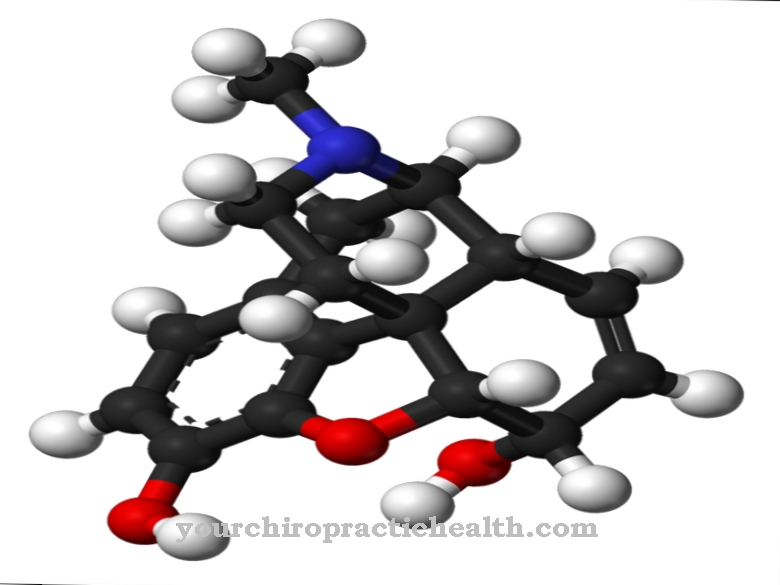
In this case, a hydrogen atom accepts an electron and thereby receives a negative electrical charge. The actual reaction takes place at the active center of the enzyme. When the dehydrogenase cleaves the hydrogen anion from a substrate, cofactors take in the electrons and the hydrogen. Cofactors are molecules that play a helping role in enzymatic processes, but are not involved in the cleavage itself. The cofactors of dehydrogenases include nicotinamide adenine dinucleotide (NAD +) and flavin adenine dinucleotide (FAD).
In contrast to dehydrogenases, dehydratases split off entire water molecules from their substrate. Dehydrogenases can also cause the counter-reaction and contribute to reduction instead of oxidation. During reduction, a particle accepts electrons instead of giving them up. Biology assigns dehydrogenases to oxide reductases. These types of enzymes exist in every living organism.
Function, effect & tasks
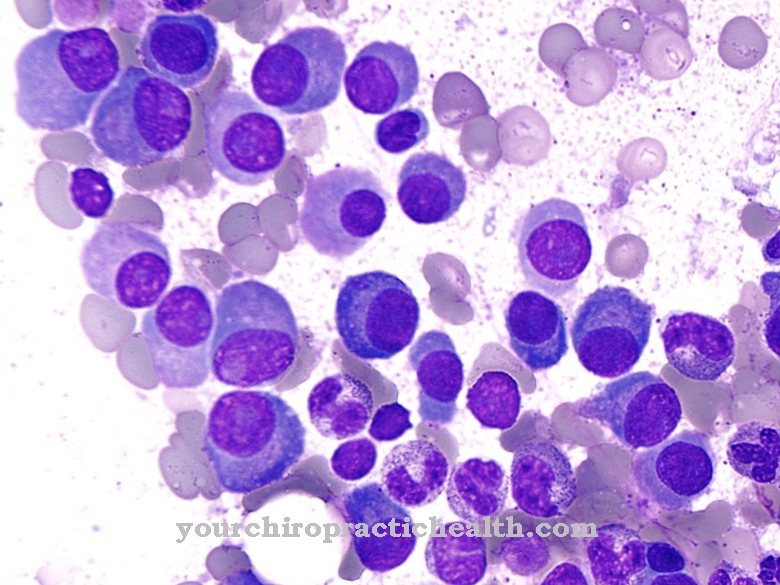
Dehydrogenases are a group made up of numerous specialized enzymes. The individual enzymes have different tasks in the human body. Biology divides the various dehydrogenases into further subgroups.
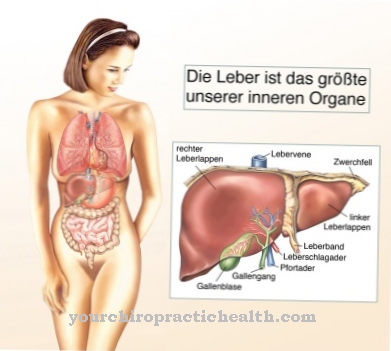
Aldehyde dehydrogenases (ALDH), for example, form a group of dehydrogenases that are mainly found in the liver. As a rule, an ALDH is only responsible for a certain substrate and cannot contribute to the oxidation of other substrates. For example, ALDH1A1, -1A2 and -1A3 process retinal, which is found in vitamin A. There are, however, exceptions to this rule: ALDH2, for example, can work with different substrates and is not limited to one substance.
In the liver, dehydrogenases break down alcohol, for example ethanol. They help cleanse the blood, which is one of the most important tasks of the liver. The ethanol molecule first docks to the active center of an alcohol hydrogenase (ADH). With the help of the enzyme, the ethanol oxidizes by splitting off the negatively charged hydrogen atom and giving it to its cofactor NAD +: In this way, ADH converts ethanol into acetaldehyde. Acetaldehyde, or ethanal, is toxic and causes a number of health ailments.
Food normally only contains a small amount of ethanol, which the body can convert quickly. Therefore the ethanal amounts are only small. The acetaldehyde in turn is the substrate for ALDH. ALDH catalyzes the conversion of acetaldehyde into acetic acid before the acetic acid can be further split and broken down into water and carbon dioxide. In this form, the molecules are completely harmless.
Education, occurrence, properties & optimal values
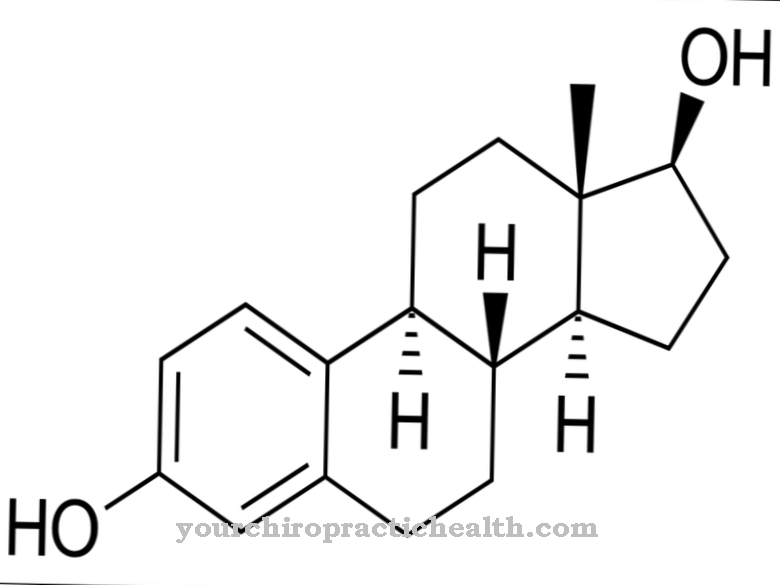
The dehydrogenases are mostly located in the liquid parts of the cell plasma or in the mitochondria. Women's bodies produce less ADH than men's bodies. This contributes to the fact that women are on average more sensitive to alcohol.
The exact values of the different dehydrogenases vary not only between different enzyme groups, but also between different individuals and ethnic groups. In East Asia and among the indigenous peoples of America and Australia, the levels of ADH are on average lower than, for example, in Europeans. The human genome has 19 known genes that determine ALDH. These genes are on the twelfth chromosome. They determine which order the amino acids take within protein chains.
The properties of the protein structures result from this sequence. The shape of the dehydrogenases and thus their function also depends on the sequence of the amino acids during synthesis. For example, ALDH2 consists of 500 amino acids. As a rule, the cells synthesize dehydrogenases, which they later also need; The transport of the substances is therefore no longer necessary.
Diseases & Disorders
When alcohol is broken down in the human body, acetaldehyde is formed as an intermediate stage. The substance is poisonous; the enzyme ALDH therefore has to convert it into acetic acid as quickly as possible. With larger amounts of alcohol, however, this usually does not work completely. Therefore, the hangover lingers a few hours after consuming alcohol.
Medicine also calls it Veisalgia. Typical symptoms are headache, malaise, queasiness in the stomach, vomiting, and loss of appetite. The ability to concentrate and react is often limited. How sensitive people are to alcohol depends, among other things, on how many dehydrogenases the liver cells produce. Dehydrogenases also play a role in the development or maintenance of various diseases. Fatty aldehyde dehydrogenase (FALDH), for example, plays a central role in the development of Sjogren's syndrome.
The main symptoms of the clinical picture are mental retardation and progressive spastic paraplegia. Spastic paraplegia is a neurodegenerative disease and is characterized by spastic paralysis in the legs. The Sjögren-Larsson syndrome also means that the horny layer of the skin is more pronounced and forms clearly visible skin flakes (ichthyosis). In addition to these three cardinal symptoms, disorders of the retina are common. The cause of the syndrome lies in the genes that code for FALDH. Due to a mutation, the body does not correctly synthesize the enzyme complex with FALDH. As a result, the concentration of fatty alcohols and fatty aldehydes in the blood plasma increases.