At a Enterocolitis there is a simultaneous inflammation of the small intestine and large intestine. A distinction is made between different forms.
What is enterocolitis?

© Romario Ien - stock.adobe.com
From enterocolitis or Colenteritis doctors speak when inflammation occurs in both the small intestine and the large intestine. Inflammation of the small intestine is called enteritis, while inflammation of the large intestine is called colitis. With enterocolitis, it is important to distinguish between infectious and non-infectious forms.
While infectious enterocolitis is caused by pathogens such as bacteria, viruses, fungi and parasites, non-infectious forms are mainly caused by other causes that are not always known. The most common infectious enterocolitis include pseudo-membranous enterocolitis, Yersinia enterocolitis and staphylococcal enterocolitis.
Among the non-infectious enterocolitis, the necrotizing enterocolitis, which occurs in babies, is known. Other forms are eosinophilic enterocolitis and regional enterocolitis, which is better known as Crohn's disease.
causes
The causes of enterocolitis vary and depend on what triggered the inflammation. This is how infectious enterocolitis develop from certain pathogens. Usually these are bacteria. The pseudomembranous enterocolitis is caused by the bacterial species Clostridium difficile.
This strain of bacteria reproduces preferentially after prolonged treatment with antibiotics. The clostridia can multiply because the antibiotic agents also kill parts of the beneficial intestinal flora. When colonizing the intestine, the clostridia give off toxins, which then lead to an inflammatory reaction. The process is similar in staphylococcal enterocolitis.
Other bacterial triggers for enterocolitis include Yersinia, Escherichia coli, Shigella and Salmonella. Viruses can also cause enterocolitis. These primarily include adenoviruses and enteroviruses. The same applies to yeasts such as Candida species and parasites such as Entamoeba histolytica and Giardia lamblia.
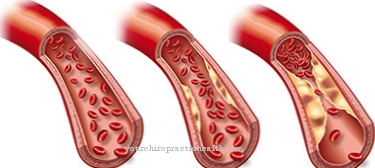
Non-infectious enterocolitis such as necrotizing enterocolitis (NEK) represent a special case. However, the exact trigger of the necrotizing form has not yet been determined. It is assumed that previous damage to the intestinal wall is responsible for local ischemia with bacteria. The germs then lead to inflammatory changes.
In addition, risk factors such as epidural anesthesia, volume deficiency shock, blood pressure that is too low and heart defects play a certain role in the development of the disease. Necrotizing enterocolitis occurs in around 12 percent of all premature babies and two percent of all newborn children.
Symptoms, ailments & signs
The symptoms of enterocolitis can vary widely, depending on how the disease originated. In all forms, however, cramping pain occurs in the abdomen. The affected people also suffer from diarrhea, which is often bloody, as well as nausea and vomiting. Furthermore, there is a general feeling of illness.
Bloody diarrhea is particularly evident in infections with Shigella, Campylobacter and amoeba. Infectious enterocolitis usually results in chills, feelings of weakness and fever. Enterocolitis caused by clostridia usually sets in two to ten days after treatment with antibiotics.
Those affected suffer from mushy, watery and bloody diarrhea, which is accompanied by intestinal cramps. In the worst case, there is a risk of an intestinal rupture, which in turn can cause life-threatening blood poisoning. Electrolyte imbalance and hypoproteinemia are also possible.
In the case of necrotizing enterocolitis, the child's abdomen expands and enlarged loops of intestine become visible below the abdominal wall. The baby can no longer tolerate the food and vomits bloody gastric juice. In the further course there is a threat of life-threatening blood poisoning.
diagnosis
To diagnose enterocolitis, the doctor needs a detailed medical history of the patient. Important criteria are the occurrence and duration of the illness as well as the use of drugs and possible concomitant illnesses. Most enterocolitis are caused by certain pathogens.
For this reason, the microbiological examination of a stool sample must be carried out. Since the patient also loses a lot of electrolytes and fluids, these factors are checked by blood tests in a laboratory. A colonoscopy is a sensible method of examination if regional enterocolitis is suspected or if it is chronic.
To diagnose necrotizing enterocolitis, an X-ray examination and sonography (ultrasound examination) are performed. The course of the necrotizing form depends on how quickly therapy is started. If the blood poisoning can be brought under control with drugs, the prognosis is considered to be relatively favorable. However, death occurs in around five to ten percent of all sick babies.
When should you go to the doctor?
If you suddenly notice severe gastrointestinal complaints, fever, chills and other signs of enterocolitis, you should consult a doctor without delay. If serious complications such as bowel cramps, bloody diarrhea or symptoms of blood poisoning become noticeable, this requires immediate clarification and treatment by an emergency doctor. If the fever increases and signs of electrolyte imbalance or hypoproteinemia, it is best to take the person to hospital.
Parents who notice a bloated abdominal wall and vomiting in their child should consult the emergency medical service. A medical evaluation and treatment is always required for enterocolitis. People who experience the symptoms mentioned after prolonged antibiotic therapy should speak to their doctor.
People who have previously had another bacterial disease are also prone to colon and small intestinal inflammation and should see a doctor immediately. In addition to the family doctor, a gastroenterologist or an internist can also be visited. In the event of a medical emergency, the emergency services must always be called in.
Doctors & therapists in your area
Treatment & Therapy
Treatment for enterocolitis depends on the underlying cause. If it was caused by clostridia, the antibiotic responsible must be discontinued or changed. In severe cases, the patient is given medication such as metronidazole or vancomycin for about two weeks. However, relapses can occasionally occur.
If the enterocolitis is uncomplicated, it is usually sufficient to treat the symptoms and give the patient sufficient fluids and electrolytes. With autoimmune enterocolitis, immunosuppressants must be administered.
In the case of necrotizing enterocolitis, the child's gastrointestinal tract nutrition should be interrupted for up to ten days and infusions should be used instead. Blood poisoning is treated with antibiotics. If it comes to an inflammation of the peritoneum (peritonitis), a surgical procedure must take place.
Outlook & forecast
Enterocolitis is a serious complication that can be treated well. If it is detected early, there is a high chance of a full recovery. The patient must change his or her diet (a feeding break is indicated for newborns) and take antibiotics. If the cause of the ailment is identified and corrected at the same time, there is a roughly 60 percent chance of recovery in the lightest birth weight group.
In the heaviest birth weight group, around 85 percent of infants survive. So the prospect of a cure is relatively good. However, enterocolitis can cause long-term health problems. The enlarged loops of the intestine can cause problems with food intake. The affected newborns often vomit and also have no more bowel movements. This can lead to constipation, anemia, and other complications, some of which are life-threatening.
In the worst case, sepsis can occur, which is often fatal for the newborn. Other possible complications are respiratory, skin and circulatory disorders. A hole can form in the wall of the intestine, which can lead to gastrointestinal problems. The prognosis depends on which of these symptoms and ailments occur and how the child reacts to the prescribed medication. In principle, however, a good to very good prognosis is possible for enterocolitis.
prevention
Preventing enterocolitis is difficult. In the case of the necrotizing form, prevention can be carried out with antibiotics. However, due to the risk of resistance, it is rarely used.
Aftercare
With enterocolitis, the follow-up activities are very limited. First and foremost, immediate treatment by a doctor is necessary to prevent further complications and, in the worst case, the death of the child. For this reason, an early diagnosis of this disease is very important.
The earlier enterocolitis is diagnosed, the better the prognosis and the better the healing of this disease. In some cases, however, this disease also reduces the life expectancy of those affected. The children are often dependent on antibiotics. It is important to ensure that the medication is taken regularly in order to completely alleviate the symptoms. It is not uncommon for part of the intestine to be removed.
The child should definitely rest after the operation, whereby the body must be spared. Refrain from exertion or other activities. The parents and relatives very often need psychological support from friends or a professional doctor. Contact with other affected parents of enterocolitis can also be useful and lead to an exchange of information.
You can do that yourself
Simultaneous inflammation of the small intestine and large intestine is a very serious condition. A patient can treat mild forms himself, since in these cases it is sufficient to supply sufficient fluids and electrolytes. However, self-treatment is not recommended, as inadequately treated enterocolitis can very quickly lead to life-threatening complications.
A person affected should promptly consult a doctor and follow his instructions. Treatment with antibiotics is often required for infectious enterocolitis. Since these drugs kill not only harmful pathogens, but also beneficial bacteria in the intestine, the result is often severe diarrhea.
Those affected can prevent these side effects by supporting the intestinal flora by consuming probiotic foods such as yogurt. Ingesting beneficial bacterial strains directly is even more effective. Corresponding preparations are available in pharmacies and health food stores.
The manufacturers of these products pack the lactic acid bacteria in gastric juice-resistant capsules so that they actually get into the intestine in large numbers and can settle there. Vaginal suppositories with lactic acid bacteria, which are available over-the-counter in pharmacies, help against antibiotic-induced colonization of the vagina with yeast.


.jpg)
.jpg)