As Flucytosine is called a pyrimidine antifungal agent. The drug is used to treat fungal diseases.
What is flucytosine?
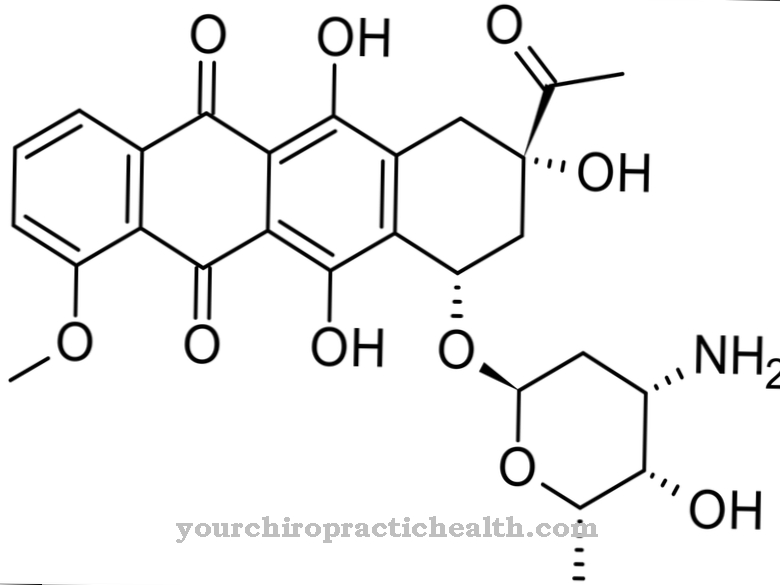
In medicine, flucytosine is also called 5-fluorocytosine, 5-FC or Flucytosinum known. What is meant by this is a heterocyclic organic compound that has a pyrimidine skeleton. The active ingredient is a derivative of the nucleobase cytosine. As a systemic antimycotic, flucytosine is used for various fungal diseases (mycoses) under the trade name Ancotil®.
Flucytosine is a so-called prodrug. This is understood to mean a little active drug that develops into an active ingredient in the course of metabolism (metabolism).
Pharmacological effect
Flucytosine is chemically related to the heterocyclic organic compound pyrimidine. The pyrimidine forms the basis for building blocks from the genetic material (DNA) and the transporting substance (RNA), which is involved in the production of proteins.
Flucytosine is absorbed in mushrooms by a special enzyme. In the further course of the process, the active ingredient is converted into 5-fluorouracil, which is incorporated into the cellular RNA. At this point, the substance can develop its effect as a "wrong building block" and ensures that the production of protein in the mushrooms is incorrect. Furthermore, the antimycotic is responsible for inhibiting the production of genetic material.
Flucytosine has a growth-inhibiting and killing effect on yeast infections such as chromomycosis and cryptococcosis. In the case of Aspergillus mushrooms, the effect is limited to inhibiting the growth of the fungus.
In principle, flucytosine can only work in the cells of fungi. In humans and mammals, on the other hand, there is no enzyme that transmits the active ingredient into the body's cells. The half-life of flucytosine is three to five hours. 90 percent of the antifungal agent is eliminated from the body through the kidneys.
Medical application & use
Flucytosine is suitable for treating fungal diseases in adults, children and babies. Fungal species such as cryptococci and candida as well as fungi that cause chromoblastomycosis are combated.
The most common areas of application of the antimycotic are systemic candidoses, in which the entire body, the urinary tract and the blood are attacked by fungi, causing spreading infections. The yeasts invade the affected person's organism from outside. There is a particular danger for high-risk patients whose immune system is weakened. In the worst case, the fungal infection can even have a fatal outcome.
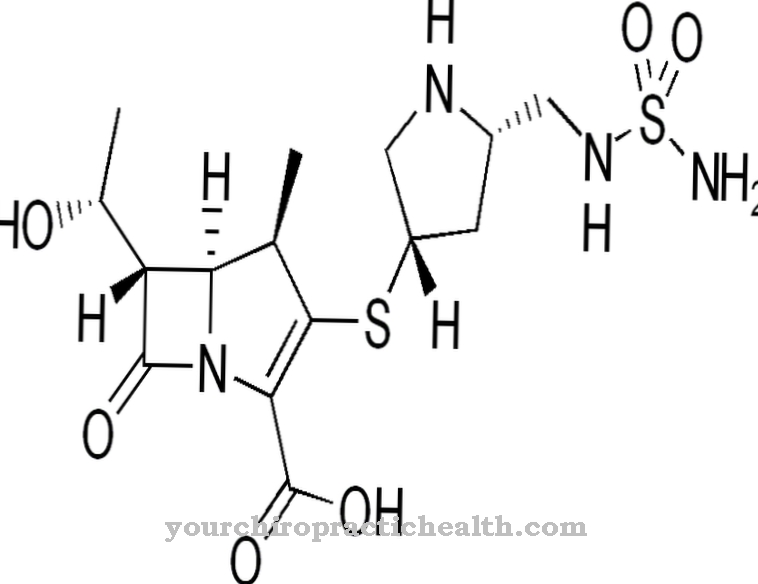
Other indications for flucytosine are meningitis caused by cryptococci (cryptococcal meningitis) and aspergillosis. In the case of treatment with flucytosine alone, doctors always administer the antifungal agent together with the agent amphotericin B. In this way, resistance can be established Avoid the pathogen against the active ingredient. If the patient suffers from cryptococcal meningitis and does not react well to amphotericin B, a combination with fluconazole can alternatively take place.
Flucytosine is administered either as an infusion solution or orally. The recommended amount of the active ingredient is 150 milligrams, which are distributed in four doses. The tolerance of the antimycotic is classified as good.
Risks & side effects
The use of flucytosine may cause side effects, but they do not automatically occur in every patient. The most common symptoms are changes in the blood count such as a lack of white blood cells, platelets and granulocytes, anemia, nausea, vomiting, diarrhea, a temporary increase in liver values and liver dysfunction.
In addition, headaches, dizziness, feelings of weakness, dry mouth, tiredness, drowsiness, breathing problems, chest pain, stomach pain, hives, rash, itching, fever, concentration problems or confusion are conceivable.
In rare cases, Lyell's syndrome, movement disorders, convulsions, psychosis, hearing loss and hallucinations occur. Even a life-threatening death of the liver cells is possible.
Flucytosine should not be administered if the patient is hypersensitive to the antifungal agent. The same applies if the patient undergoes therapy with antiviral agents at the same time, as they have an inhibitory effect on the metabolism of flucytosine, which in turn can result in poisoning. These drugs include sorivudine, ganciclovir, brivudine, and valganciclovir.
The doctor must carefully weigh up the risks and benefits in patients who are being treated with immunosuppressants or cytotoxic drugs, suffer from impaired liver or kidney function, or who are deficient in the enzyme dihydropyrimidine dehydrogenase. Due to the lack of enzymes, the flucytosine cannot be broken down properly.
The partial breakdown of flucytosine into 5-fluorouracil makes changes to the human genome possible, which can lead to malformations. Therefore, women of childbearing potential must use effective contraception during treatment. Protective measures also apply to men being treated with the antifungal agent. Flucytosine must never be used during pregnancy, as it can penetrate the placenta and damage or even kill the unborn child. It is also not recommended to use it during breastfeeding.
The simultaneous administration of flucytosine and certain other drugs can lead to interactions. This is especially true for substances that can have a negative effect on the filtration properties of the kidneys. In this case, the doctor must closely monitor the kidney functions.
A weakening of the effect of the antifungal agent is attributed to the cytostatic agent cytarabine. Basically, the simultaneous administration of flucytosine and cytostatics can lead to a shortage of blood platelets (thrombocytes) and white blood cells (leukocytes).



.jpg)




















