The Early summer meningoencephalitis (TBE) is an infectious disease caused by TBE viruses. These, in turn, are mostly transmitted by ticks or wooden rams. Since around 5% of all ticks in Germany are infected with this virus, it is advisable to get vaccinated against early summer meningoencephalitis (TBE) and to cover the whole body with suitable clothing when hiking through meadows and forests.
What is early summer meningoencephalitis (TBE)?
.jpg)
© Tatyana - stock.adobe.com
Early summer meningoencephalitis (TBE) is an inflammatory disease of the brain and spinal cord. The technical term "meningoencephalitis" is made up of the word components "Meninx" (Greek: meninges) and "Enképhalon" (Greek: brain). This meningitis occurs more frequently in June, July and August.
Baden-Württemberg and Bavaria are high-risk areas in Germany. The frequency distribution allows the conclusion, however, that early summer meningoencephalitis (TBE) is increasingly shifting northwards. According to the Infection Protection Act, cases of TBE within Germany must be reported to the health department.
causes
The early summer meningoencephalitis (TBE) is caused by the infection with the TBE virus. Infection occurs through the bite of a number of types of ticks. However, the main culprit is the wood tick, one of our most common native ticks. The parasites lurk especially in the grass and the lower herbaceous layer and cling to our body if they come into contact with them. If the animals prick the skin for a blood meal, their saliva enters the human body, which means that the viruses penetrate the bloodstream.
Not everyone who becomes infected with early summer meningoencephalitis will also get the disease. The majority of infected people who actually fall ill even have hardly any symptoms of the disease. When symptoms are felt, they resemble flu. In addition to fever, fatigue and aching limbs, neck stiffness typically occurs.
If the central nervous system is severely damaged by a disease of early summer meningoencephalitis, permanent paralysis can result. Mental performance can also be impaired. In the case of serious long-term effects, the need for care, sometimes even being completely bedridden, is the result.
Symptoms, ailments & signs
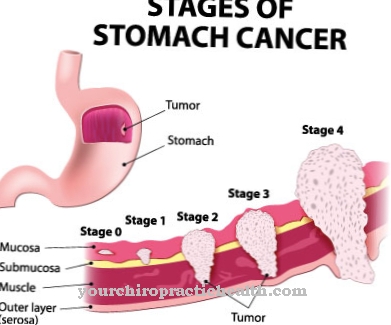
The early summer meningoencephalitis (TBE) basically runs in two phases. However, only a small proportion of those infected develop symptoms at all. In the first phase, the first symptoms appear after a few days to several weeks after being bitten by an infected tick.
There are flu-like symptoms with fever, loss of appetite, headache and body aches. These first symptoms often resolve after a short time. However, the fever may rise again after a while. After this first phase, the disease is either over or the second, more severe phase of TBE follows.
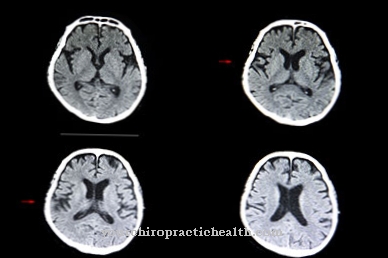
In the second phase of the disease, the TBE virus attacks the central nervous system. This can lead to inflammation of the meninges (meningitis), the brain (encephalitis) and the spinal cord (myelitis). The consequences of this inflammation are headache, nausea, vomiting and fever. Rigid neck and increasing photophobia are particularly typical of meningitis.
If the brain is affected by the inflammation, speech disorders, paralysis, epileptic seizures and changes in personality can also occur. A possible respiratory paralysis is feared. If the spinal cord is also affected, the disease spreads further. Due to its function as a central connection between the brain and the rest of the body, paralysis can now also occur on arms and legs, for example.
course
In addition to the general flu-like symptoms, the course of early summer meningoencephalitis (TBE) can also lead to more severe symptoms. Around 10 percent of those affected will develop TBE in the second phase. This can lead to complications in the form of meningitis and inflammation of the spinal cord. Paralysis related to the nervous system, epileptic seizures and other mental disorders (dizziness) can also occur.
However, these complications mostly occur in children with early summer meningoencephalitis (TBE). Older people who develop TBE, however, often tend to die from these diseases, as the symptoms and complaints put too much strain on the already old and weak body.
Complications
Complications are rarely to be feared with early summer meningoencephalitis. However, if an illness shows up, there is a chance that a second stage may appear after the first stage, which is similar to flu. In such cases, around ten percent of all patients have to expect a complicated course of the disease.
The negative sequelae often occur in the context of meningoencephalomyelitis. This is an inflammation of the brain, the meninges and the spinal cord. If TBE results in a severe course of the disease, there is a risk of permanent damage. In the worst case, even the death of the patient is possible.
About one percent of all affected people die from the severe effects of early summer meningoencephalitis. The risk of death increases with the number of nerve structures affected by the disease. In addition, there is a risk that certain functions of the body will fail for the rest of life.
One of the biggest problems of TBE is that many patients have to suffer from sequelae for months or even years after a severe course of the disease. Headache, paralysis and epileptic seizures are typical symptoms. In some cases, the symptoms take a chronic course.
Complications of early summer meningoencephalitis almost always only occur in adult patients. In contrast, children are rarely affected. However, due to the higher proportion of tick bites, the risk is rated higher in children.
When should you go to the doctor?
A doctor's visit is necessary if a tick in the skin cannot be safely removed on its own. If the tick is in an area that is difficult to access or if the person concerned feels overwhelmed by the removal, it is safer for a doctor to professionally remove the tick. If the tick could not be completely removed with independent treatment, a doctor should be consulted immediately.
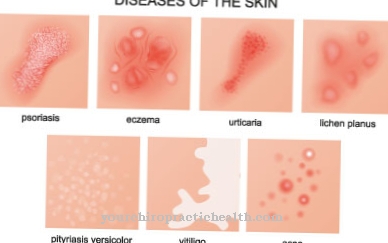
Through the remains of the animal's body, viruses can enter the organism at the site of the tick bite, which lead to early summer meningoencephalitis. Therefore, professional removal of the rest of the animal carcass is necessary as soon as possible. If there are health irregularities after a tick bite, a doctor should also be consulted. A doctor is needed in the event of general malaise, increased body temperature, dizziness or vomiting.
If there is an inflammation of the wound, reddening of the skin and noticeable swelling, these should be medically clarified and treated. If there is a diffuse feeling of pain in different parts of the body or if the person concerned suffers from diarrhea, cough and other flu-like symptoms, he should consult a doctor. In the event of a disturbance of consciousness, it is advisable to call an emergency doctor. Until it arrives, the instructions of the rescue service must be followed and calm must be kept.
Doctors & therapists in your area
Treatment & Therapy
A causal treatment of early summer meningoencephalitis (TBE) is not possible. Only the symptoms can be relieved, so the patient is prescribed pain and fever lowering drugs. Strict bed rest is also advisable. Nevertheless, if TBE is suspected, a doctor should be consulted immediately in order to rule out complications.
Outlook & forecast
In 70 to 90 percent of all cases, early summer meningoencephalitis runs without significant complications and heals without consequences. If the disease reaches the second phase, the prognosis must be made more cautious: depending on the affected area of the central nervous system, long-term consequential damage can occur. In the worst case, the disease can lead to death. Life-threatening courses mostly occur in adults, only very rarely in children.
Inflammation of the meninges is most common in the second phase of the disease. This form of TBE requires inpatient monitoring, and full recovery can take several weeks. Usually the meningitis does not cause permanent damage.
If the inflammation spreads from the meninges to the brain tissue, the prognosis deteriorates significantly. Despite intensive medical treatment, symptoms of paralysis occur in some cases, which can be life-threatening. If the patient survives the acute phase of illness, he will often suffer from motor disorders or epileptic seizures for a few months.
The recovery process is usually slow, but full healing is possible. Deaths occur predominantly in the rare myelitic form of early summer meningoencephalitis: In addition to the brain, the spinal cord is also affected. In this form, the destruction of the nerve cells can lead to respiratory paralysis and thus death.
prevention
Due to the lack of therapy options when the disease has broken out, preventive measures are particularly important in the fight against early summer meningoencephalitis (TBE). This primarily includes avoiding tick infestation. Anyone who ventures into nature, even if it is just the lawn at home, should only do so well dressed. Sturdy shoes and long trousers are compulsory, at best the trousers are tied at the ankles.
Particular care should be taken when gardening. Incidentally, it should be noted that infections with early summer meningoencephalitis are less common, even outside the main season, but are quite possible. Because the ticks become active from a temperature of 7 ° Celsius. After being outdoors, the entire surface of the skin should be searched for ticks and these should be removed immediately. Acting quickly is important! This is because animal experiments have shown that the likelihood of infection increases significantly with the duration of the tick infestation.
Pharmacies and drugstores keep special tick tongs ready to remove the parasites. The animals should either be pulled straight out or twisted out with the instrument. Pressure on the entire body of the tick must be avoided if possible.
The best protection against infection with early summer meningoencephalitis is active immunization, also known as vaccination. The doctor injects TBE viruses that have been rendered harmless, whereupon the human organism forms its own antibodies. Three vaccination sessions over the course of a year are necessary to achieve full protection against TBE. A lifelong booster immunization is required, as with other vaccinations. In the case of early summer meningoencephalitis, this should be done 3 years after the main vaccination.
Aftercare
As a rule, those affected with early summer meningoencephalitis have no direct and special follow-up options available. The patient relies primarily on medical care and treatment to prevent further complications. In general, all contact with ticks should be avoided.
When outdoors, people must protect themselves from early summer meningoencephalitis with clothing or sprays. Clothing that covers the entire body should be worn, especially in forests or meadows. Treatment for early summer meningoencephalitis is usually with medicines that lower the fever and relieve pain.
Special treatment is not necessary. It is important to ensure that these products are taken regularly and, above all, correctly in order to combat the symptoms quickly. The person concerned must also rest and take care of his body. Strict bed rest applies to early summer meningoencephalitis and all stressful and strenuous activities are not recommended.
This is the only way for the body to fully recover and combat early summer meningoencephalitis. The life expectancy of the person affected is usually not reduced by this disease. In the case of serious complaints, however, a hospital should be visited.
You can do that yourself
Due to the fact that there is no causal drug therapy for early summer meningoencephalitis, the self-help measures that infected people can initiate are limited.
There are a few things that people can watch out for that will help the body fight the infection. So bed rest is very important and should be observed. Physical and excessive mental exertion should be avoided. In doing so, one should not do without food, but rather a well-to-eat, small-portioned and balanced diet should be promoted. The fever should by no means be suppressed, provided it does not rise too high, as it fights the TBE pathogen. A warm development promotes heat development and sufficient fluid intake promotes sweating.
In addition, the person affected should be checked regularly, as this allows possible complications to be recognized at an early stage and admission to a hospital can take place in good time.
After surviving a severe infection, those affected should participate in the therapies in their everyday lives, depending on the degree of damage caused by the TBE. This also includes creating a suitable environment (for motor impairments) and should include memory games, language exercises, etc.

.jpg)






.jpg)



.jpg)










.jpg)
