Fundic varices are varicose veins in the stomach area, which are often associated with varices of the esophagus and open a bypass circuit. The cause of this phenomenon is usually a portal hypertension or a drainage disorder due to compression. In addition to preventing the bypass cycle, there is also a causal treatment of the primary disease.
What are Fundic Varices?

© matis75 - stock.adobe.com
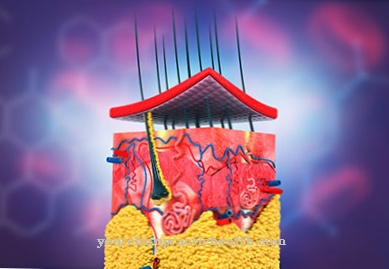
Veins divert blood from the body's periphery and transport it back to the heart, where the blood circulation and oxygenation of the blood via the arterial circulation starts all over again. The vessels of the blood circulation can fall ill with different diseases. A common disease of the veins is, for example, varicose veins.
These so-called varices are pathologically dilated veins that are visibly tortuous within the subcutaneous tissue. Varicose veins are preferably located within pressure-loaded venous areas of the lower extremities. In all other cases, they are mostly an indication of pathological bypass circuits. This is also the case with fundic varices.
This term hides intramural submucosal vein widenings in the area of the dome of the stomach. Fundus varices are often associated with varicose veins of the esophagus and in this case point to pathological processes in the abdominal cavity.
The fundic varicose veins usually affect the gastric veins. As with all varicose veins, the earlier the changes are treated, the greater the chance of success with fundic varices. Compared with varices of the legs, fundic varices are a rather rare phenomenon.
causes
The body always opens bypass circuits when individual vessels can no longer be used adequately for blood transport. This is the case, for example, with compressions or severe vascular calcification. Fundus varices also correspond to bypass circuits and represent a rare complication of various phenomena.
The bypass circuits occur, for example, in splenic vein congestion, venous compression in the spleen area or venous compression of pancreatic cancer. In addition, the appearance may indicate portal hypertension, that is, an appearance of high pressure in the portal vein.
Fundus varices open bypassing cycles and increase the volume load on the newly emerging vessels. In the case of portal hypertension, the portocaval anastomosis ensures venous drainage. In the case of bypass circuits with fundic varices, drainage occurs via the gastric veins and the downstream oesophageal veins.
Occlusions of the splenic vein achieve compensation via a short circuit with the left gastroomentalis vein. The blood travels via the superior mesenteric vein to the inferior vena cava, where it is drained.
Symptoms, ailments & signs
Most patients with fundic varices do not even notice the opening of a bypass circuit. Symptoms of fundic varices are rather rare. The clinical course corresponds to an asymptomatic course in almost all cases.
In most cases, together with the varicose veins of the dome of the stomach, those of the overlying esophagus also form, which also remain completely symptom-free. Symptoms only appear later. All symptoms are usually preceded by perforation of the bypass circuits.
This perforation often results in bleeding, which causes epigastric symptoms. From this point on, the pathological processes within the stomach usually manifest themselves in feelings of pressure and pain. Melena and hematemesis can occur.
This means that the patient may vomit blood or notice traces of blood in their stool. Blood in the stool is mainly shown as black. Depending on the causative primary disease, further symptoms may appear, for example upper abdominal pain, back pain and nausea in the case of venous compressing pancreatic cancer.
diagnosis
The clarification of fundic varices requires clear evidence of bleeding. This evidence is provided with the appropriate anamnesis via the stool sample, can include a haemoccult test, or it can be done using endoscopic measures such as gastroscopy. If the vein enlargements are confirmed on the imaging, an examination of the esophagus is carried out as part of the further diagnosis to clarify possible esophageal varices.
If the esophageal varices are also confirmed, the diagnosis of portal hypertension is obvious. In the case of isolated fundic varices, drainage disorders of the splenic vein are the more likely diagnosis. In this case, the primary disease must be clarified. To clarify the underlying disease, specific anamnesis is required, which is combined with a laboratory blood test and imaging of the individual vessels.
Imaging of the portal vein and splenic vein including the surrounding tissues is indicated. Both the livelihood and the pancreas must be examined for any tumors or cysts. In the differential diagnosis, fundic varices must be distinguished from other causes of gastrointestinal bleeding. The prognosis for patients with fundic varices depends on the primary disease.
Complications
In most cases, there are no direct complaints or symptoms due to the fundic varices. For this reason, the disease is not recognized directly and diagnosed very late. However, the symptoms show up as the disease progresses, when the varicose veins have fully developed. The affected person suffers from heavy bleeding and pain.
The pain can usually appear as pressure pain or in the form of pain at rest and extremely restrict the patient's everyday life. It is not uncommon for a bloody stool to occur, which can lead to panic attacks in many patients. Pain also occurs in the area of the abdomen and stomach, which is usually also associated with nausea.
Fundus varices can usually be treated well so that the symptoms are limited and alleviated. However, after the symptoms have subsided, causal therapy must also be carried out so that the disease does not recur and no bleeding occurs. In most cases, fundic varices do not reduce life expectancy. However, the affected person has to expose himself to further examinations after the illness.
When should you go to the doctor?
Since the onset of the fundic varices is completely symptom-free, those affected do not experience any feeling of illness or receive a warning from the body to which they could react. The first signs can only be noticed when the disease is more advanced and the fundic varices are already well developed. If the person experiences unusual pain or feels repeatedly weak for no understandable reason, this is cause for concern.
Feelings of pressure in the stomach or chest area set in, which must be examined and treated.If the initial symptoms spread continuously or the symptoms increase in intensity, it is advisable to consult a doctor as soon as possible. If changes in the appearance of the skin develop, discolouration occurs and bruises can be seen on the upper body, these should be clarified by a doctor. In the event of vomiting, diarrhea, exhaustion, palpitations or sleep disorders, a doctor must be consulted as soon as the symptoms recur.
If blood is vomited or there is blood in human excretions, it is necessary to consult a doctor. Nausea, dizziness, and back pain are other signs of irregularities that should be investigated. In the case of a general feeling of illness, circulatory disorders, internal restlessness and reduced performance, it is advisable to present the information to a doctor in order to determine the cause.
Doctors & therapists in your area
Treatment & Therapy
Varices of the esophagus are often treated by invasive procedures such as rubber band ligation. Ligatures are constrictions that prevent the bypass circuit. However, if fundic varices are associated with esophageal varices, rubber band ligation is not indicated.
This type of treatment has been scientifically proven to increase the risk of bleeding. Instead of rubber band ligation, endoscopic [[synthetic resin sclerotherapy9] is used to stop the bleeding. If the bleeding cannot be stopped massive or endoscopically, clinical treatment measures such as the installation of compression tubes are indicated.
These probes are usually Linton-Nachlass probes. Since such procedures correspond to a purely symptomatic treatment, a causal therapy of the underlying disease must also be carried out. In the case of fundic varices, this causal therapy usually corresponds to surgical excision of the masses that are present.
prevention
Fundus varices can only be prevented to the extent that the causes of bypass cycles can be prevented. At most, the preventive measures in the context of pancreatic tumors in the broadest sense can lower the risk of developing fundic varices.
Aftercare
In the case of fundic varices, the person concerned is usually not entitled to any special follow-up care options. The disease must first and foremost be treated directly by a doctor in order to prevent further complications and complaints. Self-healing cannot occur, and if left untreated, the disease can also lead to the death of the person affected.
The earlier the fundic varices are recognized, the better the further course of this disease. In most cases, those affected are dependent on a surgical procedure, which is usually carried out on an outpatient basis. Usually there are no further complications. After this procedure, the person affected should always rest and take care of their body.
Here you should refrain from exertion or stressful activities in order not to unnecessarily burden the body. Sports activities should also not be carried out. It is not uncommon for patients to have to have regular examinations by a doctor even after treatment of the fundic varices in order to prevent further complications.
The underlying disease that was responsible for the fundic varices should also be identified so that this can also be treated. It cannot generally be predicted whether the fundus varices will lead to a reduced life expectancy for the affected person.
You can do that yourself
Sufferers of fundic varices should avoid overexertion and heavy stress in everyday life. Carrying and lifting heavy objects as well as other physical excessive demands can suddenly trigger health impairments, which must be prevented.
In addition to the physical strain, the mental and emotional challenges must also be reduced. In the event of stress or strong feelings, the patient should be careful not to develop a negative attitude towards life. For your own inner relief, relaxation methods can be used to create an inner balance.
With methods such as yoga or meditation, an emotional and psychological balance can be created, which helps to relieve the organism. Controlling emotions and changing stressful cognitive patterns help the patient to develop an optimistic basic attitude. Good self-reflection is important in everyday life in order to recognize the first signs of physical irregularities and to be able to react to them.
With a healthy lifestyle and sufficient exercise, it is possible for the patient to maintain and improve their existing well-being. Obesity should be avoided and rigid postures should be avoided to prevent circulatory disorders. If pain occurs, it is advisable not to take pain medication on your own. Consultation with a doctor is necessary so that no further complications arise. In addition, autogenic training helps in dealing with pain.





.jpg)




















