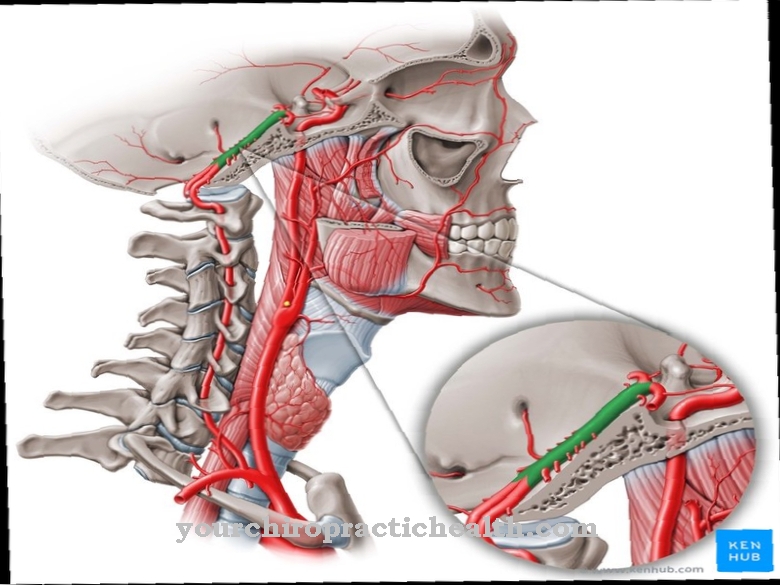
At the Pterygopalatine ganglion it is a parasympathetic ganglion. It is located at the base of the skull on the pterygopalatine fossa.
What is the pterygopalatine ganglion?
In medicine, the pterygopalatine ganglion is also called Sphenopalatine ganglion or Palatal ganglion designated. What is meant is a parasympathetic ganglion. It is located near the palatine bone (os palatinum) in the alar palatine fossa (fossa pterygopalatina) and is in front of the processus pterygoideus osis sphenoidalis (sphenoid alar process).
A ganglion is an accumulation of nerve cell bodies that belong to the peripheral nervous system. Since ganglia mostly have nodular thickenings, they are also known as nerve nodes. The functions of the pterygopalatine ganglion include the switching of parasympathetic (secretory) fibers for the palate, pharynx, nasal and lacrimal glands. The same applies to the vessels of the brain and face.
Anatomy & structure
Anatomically, the pterygopalatine ganglion is located near the sphenopalatine foramen, the maxillary nerve (maxillary nerve) and the maxillary artery (maxillary artery). The nerve node is traversed by sympathetic, parasympathetic and sensitive fibers.
An interconnection within the ganglion only takes place in the parasympathetic fibers. It only serves as a transit station for the other fibers. The parasympathetic fibers are part of the nerve cells of the nucleus salivatorius superior. Within the geniculate ganglion, it splits off from the facial nerve (facial nerve). Together with the pterygoid canal nerve and the major petrosal nerve (large temporal bone nerve), they run in the direction of the pterygopalatine ganglion. There it is connected to the postganglionic neuron.
Mainly via the branches of the facial nerve, the fibers are forwarded to their successor organs. They reach the nasal mucosa via the rami nasales posteriores superiores in the rear nasal cavity area, via the rami orbitales to the mucous membrane of the sphenoid sinuses (sinus sphenoidales) and the ethmoid cells and the ramus pharyngeus to the mucous membrane of the pharynx. Further target organs of the fibers are the nasal and palatal mucosa, which they reach via the palatine nerve, the mucous membrane of the anterior palate via the nasopalatine nerve, the soft palate via the palatine nerve and the lacrimal gland (glandula lacrimalis) via the lacrimal nerve and the Zygomatic nerve.
Sensitive fibers from the maxillary nerve are supplied to the pterygopalatine ganglion via the rami ganglionares. They run through the nerve node without being connected and have afferents from the mucous membrane of the throat, nose and palate. They too reach the pterygopalatine ganglion via the ganglionic rami.
The postganglionic sympathetic fibers of the pterygopalatine ganglion have their origin in the upper cervical ganglion (ganglion cervicale superius). They reach the nerve node via the internal carotid plexus, the deep petrosal nerve and the pterygoid canal nerve. In doing so, they run through the ganglion in the direction of the lacrimal gland.
Function & tasks
The task of the pterygopalatine ganglion is to switch parasympathetic fibers for cerebral and facial vessels as well as for the nasal, pharyngeal, palatal and lacrimal glands.
The branches emerging from the alar palatal ganglion lead towards the eye socket (orbit), nasal cavity, throat and palate. The rami orbitales, rami nasalis posteriores medialis, rami nasalis posteriores laterales, the pharyngeal nerve and the palatine nerve provide for the innervation of the mucous membrane of the nasal meatus medius and superior nasal meatus, the upper sections of the nasal septum (septum nasi), and the pharynx ), the Eustachian tube (ear trumpet) and the anterior palatal mucosa.
Also of importance are the palatal nerves (nervi palatini), from which the palatal mucosa, the palatine tonsil, the maxillary gums, the maxillary sinus (sinus maxillaris) and the meatus nasi inferior are supplied. Within the pterygopalatine ganglion, the parasympathetic fibers switch to the second neuron. This process allows the glands of the palate and nose to be secretory innervated.
Diseases
Sluder neuralgia, also known as sphenopalatine syndrome, is one of the possible diseases of the pterygopalatine ganglion. Neuralgia is considered to be the model used to explain facial nerve pain. The affected people suffer from facial pain for a maximum of 20 minutes, which can also be associated with sneezing attacks.
Facial neuralgia includes parts of the upper jaw, the palate and the inner corner of the eyelid, including the root of the nose and the eyeball. Sometimes the pain radiates into the neck or shoulder. In some cases, even one-sided paralysis of the soft palate is possible.
The Sluder neuralgia was named after the American ear, nose and throat doctor Greenfield Sluder (1865-1928), who presented the model in 1908. The laryngologist also treated the disease by injecting alcohol into the pterygopalatine ganglion. Nowadays, sluder neuralgia is considered a form of cluster headache. Sluder took the view that with some facial neuralgia there is a reflex irritation of the facial nerve fibers of the trigeminal nerve (Nervus trigeminus). However, the explanatory model is now controversial among medical professionals. However, treatment is still carried out by applying topical anesthetics to the nasal mucosa.
The pterygopalatine ganglion also plays an important role in the treatment of migraines. To treat the headache, an anesthetic such as lidocaine is introduced into the palatal ganglion via a nasal tube. It has long been suspected by doctors that the nerve knot contributes to the development of migraines. Studies have shown positive results of this treatment method, which led to a noticeable reduction in pain. Around 88 percent of all treated patients required less painkillers after therapy for the pterygopalatine ganglion, since the administration of lidocaine has the effect of a reset switch on the migraine circuitry.






















.jpg)

.jpg)
