Joint diseaseIn Germany, especially degenerative changes (wear and tear), represent the most common impairment of the musculoskeletal system. Almost every second person over the age of 45 is affected by joint pain. Medically these diseases are referred to as the Arthropathy summarized.
What are joint diseases?

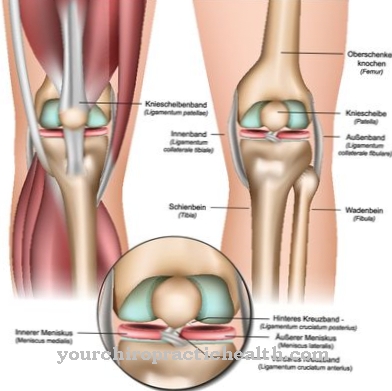
If the degenerative joint changes exceed the average age-appropriate level, it is referred to as a joint disease. The joints of the lower extremities (knee joints, hip joints) are mostly affected.
But the joints of the upper extremities (finger joints, thumb saddle joint, shoulder joint, elbow joint) can be degenerative and cause discomfort. Joint diseases belong to the spectrum of arthropathies.
These are generally divided into inflammatory (arthritis) and non-inflammatory (arthrosis) forms. In addition, a distinction can be made between infectious (reactive arthritis), inflammatory polyarthropathies (Felty syndrome, gout), arthrosis (knee joint arthrosis) and other joint diseases (protrusio acetabuli).
causes
Joint diseases are often multifactorial. The triggering factors include traumatic or growth-related misalignments (e.g.Hip dysplasia, hallux valgus, bowlegs or knock knees) as well as metabolic diseases (gout), connective tissue diseases (lupus erythematosus) and inflammatory rheumatic diseases (rheumatoid arthritis, Reiter's disease).
In addition, individual or work-related risk factors such as overweight as well as heavy physical and one-sided loads (lifting or carrying heavy loads, static muscle work, repetitive movements) can cause overuse of the joint and accelerate wear and tear. The articular cartilage increasingly has reduced elasticity and can no longer adequately compensate for mechanical loads.
This leads to the splintering of small cartilage particles into the synovial fluid. The joint is no longer adequately “lubricated”. The floating cartilage particles irritate the synovial membrane and lead to acute inflammation. The inflamed synovial membrane produces more synovial fluid. Joint effusions develop with severe pain.
The bone located under the damaged cartilage then forms so-called osteophytes (newly formed peripheral attachments) to compensate for the increased mechanical stress and hardens on the surface (subchondrial sclerosis). The normal movement pattern of the joint is impaired and the synovial membrane is additionally irritated.
You can find your medication here
➔ Medicines for joint painTypical & common joint diseases
- Osteoarthritis, arthritis, rheumatism
- Osteoarthritis of the knee
- Hip arthrosis, hip inflammation
- Joint pain
- Shoulder joint inflammation
Symptoms, ailments & signs
Joint disorders can cause different symptoms. What diseases like arthritis and osteoarthritis have in common is that they cause joint pain. Most of those affected primarily experience fatigue, start-up and stress pain. As the disease progresses, night pain and muscle pain eventually set in, which can cause secondary symptoms such as sleep problems and a general malaise.
Along with the pain, movement restrictions of the affected joints set in as the disease progresses. When moving, crunching noises occur or the typical crackling occurs. The joints become increasingly unstable and kink more often - fractures occur. Usually bony thickenings and swellings also form.
Some joint diseases (for example osteoarthritis) are expressed by externally visible joint effusions and deformities. Those affected can usually also notice muscle loss or local redness and overheating. In the later process, the bone substance thickens and deformities and deformations occur.
Joint diseases represent a considerable burden for the persons concerned, as they are mostly chronic and increase in severity over time. The physical performance decreases significantly. In the later stages, the affected joints can no longer be moved painlessly at all.
Diagnosis & course
In the early stage of the disease, a joint disease manifests itself in the clinical picture on the basis of start-up pain, fatigue and stress pain (so-called early triad). In the further course, permanent pain, night pain and muscle pain (so-called late triad) appear.
As part of the physical examination, movement restrictions, bony thickening of the joint contours, crepitation ("grinding joint movement"), instability, malpositions, muscle atrophy and contractures as well as local hyperthermia and joint effusions can be determined.
In the X-ray image, especially in the late phase, a frayed, rough surface, a narrowing of the joint space, subchondrial sclerotherapy (compression of the surrounding bone tissue) as well as pebble cysts (recesses in the bone substance) and osteophytes can be visualized.
In the case of rheumatoid arthritis, specific inflammation parameters can also be detected in the blood in the acute phase. In severe cases, pronounced joint deformation and / or secondary chondrocalcinosis (deposits of calcium pyrophosphates in the cartilage tissue) can occur.
Complications
The complications and complaints associated with joint diseases depend to a large extent on the joints affected and, for this reason, cannot be universally predicted. However, in most cases there is relatively severe pain in the affected regions and restrictions in movement. The restricted mobility can also lead to psychological complaints and depression in many people.
In addition to pressure pain, pain at rest often occurs, which complicates everyday life and reduces the patient's quality of life. Many sufferers also suffer from pain at night, which can lead to significant sleep disorders. Joint diseases can also lead to inflammation and infections. If these spread to other regions of the body, this can have serious consequences and complications.
A joint disease can also lead to the amputation of the affected limb. The treatment of joint diseases depends on the underlying disease and is carried out in most cases with the help of creams, painkillers or surgery. Therapies are also often used to relieve pain and encourage movement of the affected joints. Joint diseases usually do not change life expectancy.
When should you go to the doctor?
Joint complaints should be presented to a doctor if they do not occur immediately after a fall or accident. In addition, a medical examination is necessary as soon as the symptoms persist for several days or weeks. If they increase in intensity or if further symptoms occur, a doctor should be consulted.
If the joint disease leads to reduced drive, a loss of zest for life or if everyday obligations can no longer be carried out as usual, a visit to the doctor is advisable. A doctor must be consulted in the event of poor posture of the body, complaints of the muscles, tendons or nerves.
If there are changes in the skeletal system, pain, tension or hardening due to the joint diseases, a doctor is required. If natural movements can no longer be carried out carefree, there is a need for action.
A doctor should be consulted so that after the cause has been identified, the symptoms can be alleviated. In the case of psychological impairments, mood swings or behavioral problems, a doctor's visit is necessary. If it comes to a social withdrawal, depressive or melancholy phases and apathy, a doctor's visit is necessary.
Aggressive behavioral tendencies, choleric abnormalities or inner restlessness should be discussed with a doctor. If sleep disorders occur or if there is a lack of concentration and attention, a doctor should also be consulted. Consultation with a doctor is required before taking any pain medication.
Doctors & therapists in your area
Treatment & Therapy
The therapeutic measures depend on the underlying cause and the stage of the disease. Asymptomatic, pain-free joint diseases usually do not have to be treated. Drug therapy with non-steroidal anti-inflammatory drugs (including ibuprofen, diclofenac in the first stage) or opioids (tramadol, tilidine in the second stage) aims to reduce the pain symptoms.
In some cases, so-called chondroprotective agents (hyaluronic acid) are used. These have an anti-inflammatory effect and inhibit enzymes that have a cartilage-degrading effect. If there are joint effusions, these are usually punctured to relieve the affected joint. In the case of recurring joint effusions, a drug containing cortisone can be injected into the joint to reduce the inflammatory process over the long term.
If there is an underlying rheumatic disease, this must be treated with medication (basic rheumatoid drugs such as chloroquine, D-penicillamine). In addition, immunosuppressants (methotrexate) or tumor necrosis factor alpha inhibitors (infliximab, etanercept) can be used for chronic polyarthritis.
Occupational therapy and orthopedic measures aim to convey activities that are gentle on the joints, avoid improper strain and relieve the affected joint through forearm supports, cushioning and / or corrective insoles or shoe adjustments.
With the help of physiotherapy measures, the cycle of muscle breakdown, increasing pain symptoms, decrease in muscle activity and further reduction in muscle size, which is characteristic of joint diseases, is to be broken. Particularly in the early stages, an improvement in the degeneratively changed joints and surrounding soft tissues can be achieved by increasing joint mobility, stretching shortened muscle and ligament structures and building up muscles.
In chronic pain, electrotherapy (short wave, galvanization) can relieve pain and relax the surrounding tissue. In addition, various surgical therapy methods can be used. The joint can be rinsed and the cartilage smoothed as part of an arthroscopy (joint mirroring). Cell transplants and cartilage bone transplants can repair small cartilage defects.
Congenital or traumatic malpositions are treated with an operative axis correction in order to avoid or inhibit arthrotic processes. If there is pronounced joint destruction with permanent pain symptoms and restricted mobility, an artificial joint implantation (especially knee and hip joints) may be indicated.
Outlook & forecast
Joint diseases can have various causes. They are caused by inflammation or wear and tear on the affected joints. Knees, arms, legs, feet, shoulders or hands can be affected. If left untreated, the initially mild pain will noticeably increase. Anyone who initially only felt pain when subjected to appropriate stress, will also feel it later in the resting state. There is also pain when sitting or lying down. Movement disorders and impairments occur in everyday life.
Due to the large number of treatment options, the prognosis for joint diseases is generally very good. Mobility can be restored and the pain subsides. Physiotherapy, massage, chiropractic or osteopathy are just a few of the options. For advanced joint diseases with a comparatively poor prognosis, only surgery will help. Those who do not act here will hardly be able to do without pain killers, have to rely on a walking aid or later sit in a wheelchair.
Inflammations in the joints subside with appropriate treatment and the patient is pain-free again. The wear and tear of the joints is associated with great pain and cannot be cured. Treatment is always required to improve the patient's prognosis and relieve pain.
You can find your medication here
➔ Medicines for joint painprevention
Joint diseases and their progression can be prevented by minimizing individual and work-related risk factors. This includes reducing excess weight, avoiding one-sided stress on the joints, sporting activities that are gentle on the joints and strengthening the muscles that guide the joints.
Joint diseases caused by systemic diseases such as gout or rheumatoid arthritis cannot be prevented. However, early therapy can significantly slow their progression.
Aftercare
In the case of joint diseases, the options for follow-up care are severely limited in most cases. The disease itself cannot be treated, so that the symptoms can only be examined and alleviated purely symptomatically. A complete cure cannot be achieved either, since joint diseases are a natural state of the body that cannot be avoided in old age.
In general, a healthy lifestyle with a healthy diet and physical activity have positive effects on and can alleviate joint diseases. Sports activities are also recommended in old age in order to move the affected muscles and joints. It is also helpful to take medication to alleviate the symptoms of joint diseases and to stabilize the joints and bones.
The person concerned should always pay attention to regular consumption and possible interactions. The symptoms can also be alleviated with the help of physiotherapy, whereby the exercises from this therapy can often be repeated at home in order to increase the mobility of the body. As a rule, the joint disease does not have a negative effect on the life expectancy of the person affected.
You can do that yourself
Which self-help measures those affected can take with joint diseases depends on the cause.
The best form of self-help for degenerative joint diseases is prevention. First of all, a person affected should identify and control both individual and work-related risks in good time. The first group includes, for example, being very overweight, chronic lack of exercise or, on the contrary, excessive physical activity that puts a lot of strain on the joints.
In the workplace, regulations for work safety, especially for lifting heavy loads, should be strictly observed. Work breaks that are used to loosen up the affected muscles are very important for activities with one-sided joint stress. At the first signs of pathological wear and tear on the joints, a specialist, preferably an orthopedic surgeon, must be called in immediately. Targeted treatment in conjunction with physiotherapy can usually stop the progression of the degenerative processes.
In the case of systemic diseases of the joints, such as gout, a change in lifestyle, especially diet, can help.
Those affected who suffer from acute joint pain often benefit from temperature stimuli, with some patients reacting positively to warmth and others to cold. Those who respond positively to heat can irradiate the affected joints with red light or bathe them regularly in warm salt water. If the cold is good for you, you can use ice compresses from the pharmacy.
↳ More information: Home remedies for joint pain

.jpg)

.jpg)









.jpg)




.jpg)


