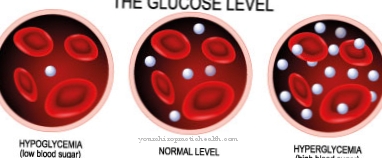
At a Glucose-6-phosphate dehydrogenase deficiency it is a hereditary deficiency of the enzyme glucose-6-phosphate dehydrogenase, which plays an important role in sugar metabolism. The symptoms of the deficiency are very variable, and in severe cases the red blood cells can be destroyed in the form of hemolysis. The disease is easily manageable by avoiding certain foods and drugs.
What is Glucose-6-Phosphate Dehydrogenase Deficiency?

© photo4passion.at - stock.adobe.com
The glucose-6-phosphate dehydrogenase deficiency indicates a deficiency or incorrect functioning of the enzyme glucose-6-phosphate dehydrogenase. The consequences of this deficiency are different. The symptoms vary from lack of symptoms to hemolytic crises. Since the disease is inherited via the X chromosome, women are usually less affected than men. This enzyme deficiency is particularly widespread in malaria areas.
Hemolytic crises are often triggered by beans (fava beans) and certain medications such as primaquine, nitrofurantoin or sulfanilamide. Because it is triggered by fava beans, the glucose-6-phosphate dehydrogenase deficiency is also known as favism when symptoms are present.
Around 400 million people worldwide are affected by this enzyme defect.Most people, mostly women, don't develop symptoms at all. As a rule, quality of life and life expectancy are not restricted with a glucose-6-phosphate dehydrogenase deficiency. Only foods and drugs that induce hemolysis should be avoided in severe forms.
causes
The cause of the glucose-6-phosphate dehydrogenase deficiency is a mutation of the G6PD gene on the X chromosome. This gene is responsible for coding the enzyme glucose-6-phosphate dehydrogenase. The severity of the symptoms depends on the specific mutation and gender of the person. Around 150 mutations of this gene are known to date. The function of the enzyme is not equally restricted with every mutation.
Girls and women have two G6PD alleles. Usually the defective gene is passed on heterozygously. So there are still enough healthy G6PD genes from the other parent. The second gene is missing in men, so that the glucose-6-phosphate dehydrogenase deficiency is more pronounced. Furthermore, the existing mutation determines the residual activity of the enzyme.
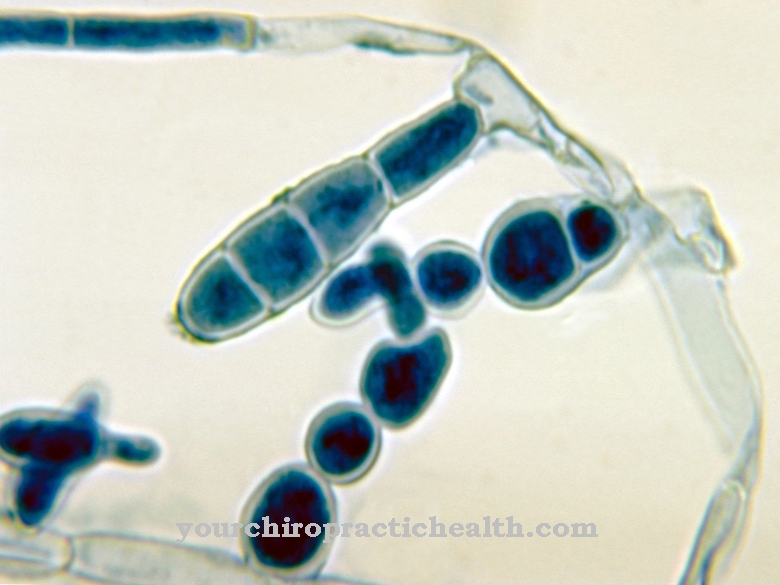
The enzyme glucose-6-phosphate dehydrogenase plays a crucial role in carbohydrate metabolism. It is responsible for converting the oxidized NADP + into the reduced NADPH. NADH in turn represents a cofactor of the enzyme glutathione reductase. Glutathione reductase reduces the dimeric oxidized glutathione to two monomers of reduced glutathione. In its reduced form, glutathione is a powerful antioxidant and scavenges free radicals.
If there is a lack of reduced glutathione, there is often insufficient capacity to destroy free radicals. This is particularly true when the addition of external substances creates a large number of radical intermediates. Fava beans, peas or currants contain certain alkaloids that cause radical breakdown products. The same applies to certain drugs. If there is too little reduced glutathione available, the free radicals are only insufficiently broken down.
Their concentration can rise to the point where they destroy the erythrocytes, causing hemolysis. The lack of reduced glutathione is in turn the result of a lack of NADH. Since the formation of NADH is catalyzed by glucose-6-phosphate dehydrogenase, insufficient activity of this enzyme also leads to insufficient regeneration of NADH from NAD +.
Symptoms, ailments & signs
A glucose-6-phosphate dehydrogenase deficiency manifests itself in different ways. Three different forms of expression are roughly distinguished. So there is a symptom-free form of enzyme deficiency. In these cases, there are still enough active enzymes available to compensate for the deficiency.
A second form is acute hemolytic anemia, which is caused by fava beans, sulfonamides, vitamin K, naphthalene or acetylsalicylic acid. Chronic hemolytic anemia, in which red blood cells permanently die, is the least common. The formation of new blood cells cannot fully compensate for their breakdown here. If the symptoms are pronounced, chills, fever, weakness, shock, back pain or abdominal pain occur, among other things.
The urine turns black. Jaundice also occurs. Neonates with glucose-6-phosphate dehydrogenase deficiency may suffer from neonatal jaundice. In rare cases, the kidneys can even fail completely. In general, compensatory processes take place in the body, so that the hemolytic crisis is quickly over. The prognosis for the disease is good. In rare cases, however, a fatal outcome is also possible.
diagnosis
To diagnose a glucose-6-phosphate dehydrogenase deficiency, the doctor will first take an anamnesis of the medical history. If symptoms such as anemia, jaundice and haemolytic features occur, there is a suspicion of glucose-6-phosphate dehydrogenase deficiency in certain ethnic groups and people who have already had cases of the disease in their relatives.
Furthermore, laboratory tests for liver enzymes, reticulocyte count, lactate dehydrogenase, haptoglobin or an immediate antiglobin test (Coombs test) are carried out. If an immunological cause for the hemolysis is excluded in the Coombs test, the suspicion of a glucose-6-phosphate dehydrogenase deficiency is reinforced.
NADH can be determined directly via the so-called Beutler test. If no fluorescence of the blood cells is observed, it means a positive Beutler test. In this way the diagnosis of glucose-6-phosphate dehydrogenase deficiency can be confirmed.
Complications
The glucose-6-phosphate dehydrogenase deficiency does not always have to lead to complications or symptoms. So the deficiency occurs even if there are active enzymes. If this is not the case, however, the glucose-6-phosphate dehydrogenase deficiency can also lead to the death of the red blood cells. This death has relatively serious consequences and symptoms that are similar to those of a common febrile illness.
This leads to fever, body aches and chills. The abdomen and back can also be affected by pain, so that the patient is severely restricted in everyday life. The quality of life decreases drastically due to the glucose-6-phosphate dehydrogenase deficiency. In the worst case, kidney failure can occur, which can even lead to death.
Infants can also develop jaundice due to the deficiency. If the glucose-6-phosphate dehydrogenase deficiency is triggered by a drug or a food, the person concerned must stop using it. In most cases, there are no further complications. A causal treatment is not possible. If the deficiency can be remedied, there is no reduction in life expectancy.
When should you go to the doctor?
People who have relatives in their family who have a glucose-6-phosphate dehydrogenase deficiency should have a genetic test carried out for clarification. If symptoms such as chills, body aches or fever occur, there is cause for concern.
The flu-like symptoms need to be controlled by a doctor. If the symptoms persist for several days, a doctor must be consulted. General weakness, back pain, or abdominal pain should be evaluated and treated.
A doctor should clarify increased tiredness, exhaustion or restlessness. If a shock occurs, a doctor should be consulted immediately. In severe cases, an ambulance service must be informed. The instructions of the emergency personnel must be followed until it arrives. Discoloration of the urine is considered unusual. If it turns black, a doctor must be consulted as soon as possible.
A doctor's visit is also necessary if the skin is yellow. If you experience kidney problems, a check-up visit with a doctor is recommended. If there are functional disorders of the kidneys, pain or a reduction in performance, a doctor is required. If fluid intake is refused due to the symptoms, a doctor's visit is required as there is a risk of dehydration. In the event of kidney failure, an emergency doctor must be called. There is a mortal danger for the person concerned.
Doctors & therapists in your area
Treatment & Therapy
There is currently no causal therapy for glucose-6-phosphate dehydrogenase deficiency. A blood transfusion may be necessary in acute haemolytic anemia. Otherwise, the therapy consists in avoiding foods and active substances that can trigger favism.
These include beans (mainly fava beans), peas, currants, vitamin K, acetylsalicylic acid, sulfonamides, naphthalene and aniline derivatives. If these triggers are avoided, there will be no symptoms. Life expectancy is not reduced with a glucose-6-phosphate dehydrogenase deficiency.
Outlook & forecast
Glucose-6-phosphate dehydrogenase deficiency is a genetic disease. Since human genetics cannot be changed for legal reasons, there is no prospect of a cure for the disorder. Therapy is therefore geared towards relieving symptoms.
In a large number of patients, despite the diagnosed disease, no impairment occurs. You will not experience any abnormalities or complaints in the course of their life. The prognosis for them is therefore very favorable and treatment is not necessary.
However, the person affected should have regular check-ups so that changes or peculiarities can be reacted to as quickly as possible. Normally, the focus of medical care is on reducing the symptoms that arise as a result of the deficiency.
The prognosis is favorable if the patient adheres to certain guidelines. A well-designed treatment and therapy plan aims to improve health. If the patient follows a special diet plan, the symptoms are significantly alleviated. The intake of certain foods should be avoided as a matter of priority.
In particular, beans, peas or currants should be removed from the diet for a good prognosis. If they are consumed, the irregularities increase again in a short time. The diet must be adhered to for life in order to increase the patient's well-being and promote the health of the patient.
prevention
Since the glucose-6-phosphate dehydrogenase deficiency is hereditary, there is no way of preventing it. Only the symptoms of hemolytic anemia can be prevented by avoiding triggering substances.
Aftercare
In the case of glucose-6-phosphate dehydrogenase deficiency, special follow-up options are usually not possible and also not necessary. The person concerned is primarily dependent on the direct treatment of this complaint in order to prevent further complications. An early diagnosis in particular has a very positive effect on the further course and can help to alleviate the symptoms.
This disease often does not have a negative impact on life expectancy. In the case of glucose-6-phosphate dehydrogenase deficiency, the patient has to rely on medication and other supplements to alleviate the symptoms. Active ingredients that trigger the symptoms should also be avoided as far as possible in order to protect the body. When taking the medication, ensure that it is taken regularly.
Possible interactions with other medications must also be taken into account, whereby the doctor can also be asked for advice. The doctor can also provide the person with a nutrition plan to guarantee a proper diet.
If the symptoms of glucose-6-phosphate dehydrogenase deficiency become severe, it is better to call an emergency doctor or go to the hospital directly. Contact with other people affected by glucose-6-phosphate dehydrogenase deficiency can also be useful, as this leads to an exchange of information that can be helpful for everyday life.
You can do that yourself
In most cases, glucose-6-phosphate dehydrogenase deficiency can be treated relatively well by avoiding certain foods. This can limit most complaints so that direct medical treatment is not always necessary. However, a nutrition plan that can also be created with a nutritionist is always suitable.
In an acute emergency, the glucose-6-phosphate dehydrogenase deficiency is usually compensated for by a blood transfusion. In the further course, the person affected should avoid beans and peas in their food. Currants or vitamin K also have a negative effect and can promote the disease. The patient should also not take aspirin or aniline derivatives. If these ingredients and foods are avoided, the symptoms of glucose-6-phosphate dehydrogenase deficiency can be completely treated.
In many cases, contact with other patients with the disease also has a very positive effect on the further course, which can lead to an exchange of information. With a strict diet, the symptoms do not recur, so blood transfusions are not necessary. As a rule, avoiding the triggering foods does not have a particularly negative effect on the patient's quality of life.


.jpg)








.jpg)




.jpg)


