The Glycogenolysis serves the organism to provide glucose-1-phosphate and glucose from the carbohydrate storage form glycogen. A lot of glycogen is stored in the liver and skeletal muscles in particular. Among other things, the blood sugar level is also influenced by the glycogen metabolism in the liver.
What is Glycogenolysis?

Glycogenolysis is characterized by the breakdown of glycogen into glucose-1-phosphate and glucose. This produces around 90 percent glucose-1-phosphate and ten percent glucose. Glycogen is the storage form of glucose, similar to what starch is in plants.
It appears as a branched molecule, in whose chains the glucose units alpha-1-4 O-glycosidically are linked to one another. At the branching point there is an alpha-1-4 O-glycosidic bond as well as an alpha-1-6 O-glycosidic bond.
Glycogen is not completely broken down. The basic molecule always exists. Either new glucose molecules are glycosidically bound to this or split off. Effective energy storage is only possible in the form of this tree-like, branched molecule.
Glycogen is present in all cells and is therefore directly available for energy supply. However, it is stored in the liver and in the skeletal muscles in order to guarantee the energy supply for a certain transitional period even when there is no food. If necessary, it is mainly broken down into the intracellular form glucose-1-phosphate. To regulate the blood sugar level, free glucose is increasingly formed in the liver through enzymatic reactions.
Function & task
Glycogenolysis provides the organism with energy in the form of free glucose and the phosphorylized form of glucose. For this purpose, the carbohydrate storage form glycogen is broken down. Since there is glycogen in all cells of the body, glycogenolysis takes place everywhere.
Glycogen is also stored in the skeletal muscles and in the liver. In this way, the high energy requirements of the skeletal muscles can be met quickly even when there is no food. The liver also ensures that there is sufficient glucose available to regulate blood sugar levels. An additional enzyme, glucose-6-phosphatase, is available in the liver to convert glucose-1-phosphate into glucose-6-phosphate. Glucose-6-phosphate can then be added to glycolysis, i.e. the formation of glucose.
The first steps in glycogenolysis are basically the same in the skeletal muscles and the liver. The alpha-1-4 O-glycosidic linked glucose molecules in the chains of the tree-like branched molecule glycogen are split off by the enzyme glycogen phosphorylase. The glucose molecule that is split off is connected to a phosphate residue. The result is glucose-1-phosphate, which can be used immediately to generate energy or to transform it into other biomolecules.
This cleavage process only takes place up to the fourth glucose unit of the chain before the branching point. The so-called debranching enzyme (4-alpha-glucanotransferase) is used to split the remaining glucose units. This enzyme does two things. On the one hand, it catalyzes the separation of three of the four glucose units before the branching point and its transfer to a free, non-reducing end of the glycogen. On the other hand, it catalyzes the hydrolysis of the alpha-1-6 branching point, which creates free glucose.
Due to the ratio of chains and branching points in the glycogen, this process only ever produces ten percent free glucose. However, even larger amounts of free glucose are formed in the liver. As already mentioned, the liver has an additional enzyme (glucose-6-phosphatase) which catalyzes the isomerization of the molecule glucose-1-phosphate into glucose-6-phosphate.
Glucose-6-phosphate can easily be converted into free glucose. In this way, the liver ensures that the blood sugar level remains constant when there is no food. If the blood sugar level falls due to physical stress or food abstinence, the hormones glucagon and adrenaline are increased. Both hormones stimulate glycogenolysis and thus ensure a balanced blood sugar level.
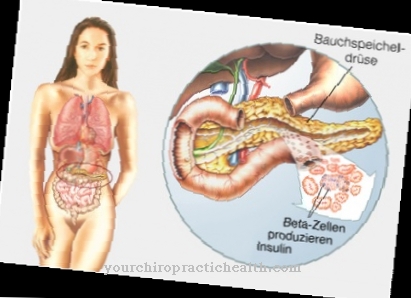
Glucagon is the antagonist of the hormone insulin, which is increased when the blood sugar level is high. Insulin inhibits glycogenolysis.
Illnesses & ailments
If glycogenolysis becomes more severe, it can be a symptom of a pathological process. The hormone glucagon stimulates glycogenolysis directly by activating a G protein-coupled receptor (GPCR). As a result of the reaction cascade that starts, a glycogen phosphorylase (PYG) is catalytically activated. The glycogen phosphorylase in turn catalyzes the formation of glucose-1-phosphate from the cleavage of glucose units from glycogen.
With an increased concentration of the hormone glucagon, there is an increased breakdown of glucogen. The bottom line is that larger amounts of glucose are created, leading to increased blood sugar levels. Strongly increased concentrations of glucagon occur in the so-called glucagonome. The glucagonoma is a neuroendocrine tumor of the pancreas that continuously produces enormous amounts of glucagon. The glucagon plasma level can be increased up to 1000 times the norm.
Symptoms of the disease are diabetes mellitus, due to the increased glycogenolysis, extremely destructive eczema on the face, hands and feet, and anemia. The tumor is usually malignant. Treatment consists of its surgical removal. If there are metastases or inoperability, chemotherapy is carried out.
With the increased formation of adrenaline, too, more glucogen is broken down. Adrenaline is produced in high concentrations in a pheochromocytoma, among other things, without the hormone level being able to be regulated. A pheochromocytoma is hormonally active tumors of the adrenal medulla. The causes of these tumors cannot usually be determined. In the majority of cases, however, it is benign tumors, which can, however, also become malignant.
In addition to high blood pressure and cardiac arrhythmias, the blood sugar level is greatly increased due to the increased glycogenolysis. Nonspecific symptoms are headache, sweating, paleness, restlessness, fatigue and leukocytosis. Therapy consists mainly of the surgical removal of the tumor.