A Hemolysis or Hemolytic anemia is a destruction of the red blood cells caused by a multitude of possible causes, which is difficult to prevent and treat and, in severe cases, can often lead to death.
What is Hemolysis?

© StockPhotoPro - stock.adobe.com
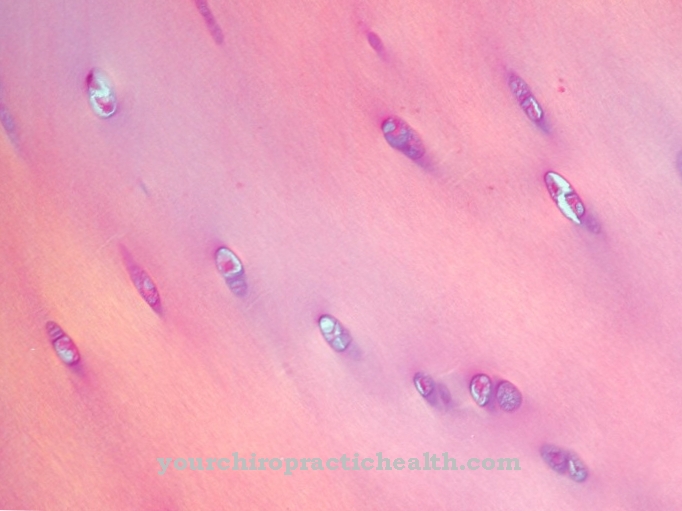
At a Hemolysis is a disease that causes red blood cells called erythrocytes to break down.
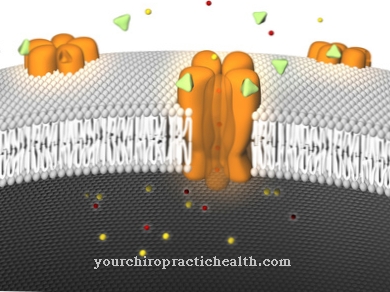
By damaging the cell membrane of the erythrocytes, the hemoglobin, which is the pigment in the red blood cells, passes into the actually colorless plasma. A distinction is made between so-called physiological hemolysis and increased hemolysis.
In the first case it is a natural death of the erythrocytes after 120 days. The second case describes an increased dissolution of the erythrocytes, which goes beyond the natural erythrocyte circulation and must be regarded as pathological.
causes
The causes of a Hemolysis are diverse. Occurring hemolysis can be a symptom of another underlying disease or it can also occur through mechanical processes or it can be genetic.
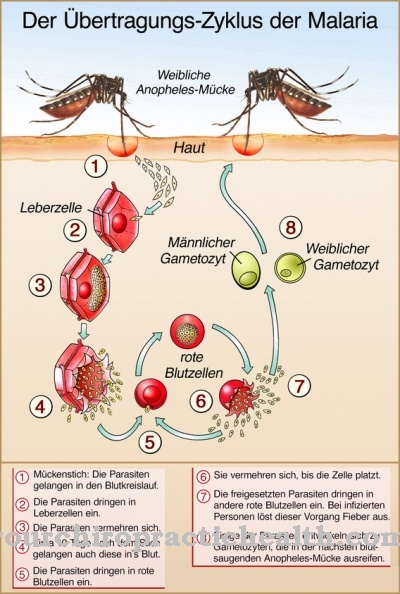
Haemolysis can occur as a result of severe infections and autoimmune diseases, as well as poisoning, heart valve prostheses and burns or defects in the erythrocyte membranes or hemoglobin. Parasites can also be a possible cause of increased hemolysis.
The first indication of a pathological hemolysis is a brown discolored urine. The discoloration is due to the fact that with increased hemolysis, more hemoglobin is excreted in the urine (see also blood in urine). A doctor may perform various tests if increased hemolysis is suspected.
If an increased number of young erythrocytes can be found in the blood with a simultaneous lower concentration of hemoglobin, this is another indication of possible hemolysis. So-called Coombs tests help to reliably diagnose a disease. However, increased hemolysis is not always recognized immediately.
Symptoms, ailments & signs
The classic symptoms of hemolysis include tremors, tiredness, poor concentration, headache, dizziness and shortness of breath, right through to rapid heartbeat during exercise. The characteristic paleness of the skin is accompanied by other symptoms of jaundice. Abdominal pain, fever and a general malaise occur, often accompanied by severe exhaustion.
Many patients also develop chills and headaches. If a hemolytic crisis occurs, symptoms such as severe stomach pain, high [[fever9] and 8 [circulatory problems]] can occur. In severe cases, circulatory collapse occurs. Gallstones often form and the spleen enlarges, which can add further symptoms. If the course is severe, thrombosis develops or kidney failure occurs.
Haemolytic anemia can also occur and is manifested by the typical signs of anemia. If the hemolysis is inadequately treated, it may lead to a loss of consciousness. The symptoms usually appear a few days to weeks after the causal disease and persist for months or even years. In some patients, symptoms resolve on their own once the trigger has been resolved. In other cases the hemolysis is fatal.
Diagnosis & course
As a result of an increased Hemolysis Various complications can arise: As a comparatively harmless cause, gallstones can occur due to hemolysis. In the worst case, however, thrombosis, kidney failure or hemolytic anemia can occur.
In this case, in contrast to a healthy body, which is able to constantly reproduce new erythrocytes, so that in physiological hemolysis the number of erythrocytes in the blood remains constant, more erythrocytes are destroyed than can be reproduced.
In the further course there may be an insufficient oxygen supply to the tissue. Due to the many possible complications, hemolysis can in not a few cases become chronic and even lead to death.
Complications
In the worst case, hemolysis can lead to patient death. The red blood cells are destroyed, so that there are various complaints and restrictions. The person concerned feels sick and tired and suffers from severe exhaustion. Jaundice can also occur, in which the patient also suffers from fever and abdominal pain.
The affected person may lose consciousness and complain of severe headaches and nausea. As a rule, special physical activities can no longer be carried out, so that there is a severe restriction in the patient's life. The enlarged spleen continues to lead to severe pain in the abdominal region.
In the worst case, kidney failure can develop, in which the patient is dependent on a donor kidney or on dialysis. If the symptoms are not treated, the patient usually dies. The treatment is always causal and is carried out in the form of a surgical intervention. Complications rarely arise here if the procedure is carried out early. Life expectancy can be reduced if hemolysis is treated late.
When should you go to the doctor?
Symptoms such as fatigue, tiredness, and jaundice suggest hemolysis. If these signs appear for no reason and do not go away on their own, medical advice is needed. Patients who suddenly have gallstones or signs of an enlarged spleen should see a doctor. If external symptoms such as paleness and sunken eyes become noticeable, the family doctor must be consulted. If there are any signs of a hemolytic crisis, such as fever and abdominal pain, the emergency doctor is the right contact.
The same applies to kidney failure, thrombosis or hemolytic anemia. Hemolysis is caused by severe infections and autoimmune diseases. Poisoning, burns or autoimmune diseases are also possible causes. Anyone who belongs to these risk groups must speak to the responsible doctor immediately if they experience the symptoms mentioned. In the event of severe complaints, it is best to go to the nearest hospital or call the emergency services immediately. Since hemolysis can recur, regular check-ups by your family doctor or an internist are advisable.
Doctors & therapists in your area
Treatment & Therapy
To a morbid Hemolysis To be able to treat efficiently, it must first be determined whether the hemolysis is a congenital form or another cause. If hemolysis is subject to another disease, the hemolysis will usually go away with treatment of the underlying disease.
For the duration of the recovery, a transfusion of red cell concentrates may be necessary in order to avoid an increase in hemolysis. If the hemolysis can be traced back to genetic causes, the treatment is often only a surgical procedure in which the spleen is removed. The same treatment is often carried out if the hemolysis has occurred because the respective immune system of the person concerned has produced antibodies that are responsible for the destruction of the erythrocytes, and drug treatment is not or no longer sufficient.
In the case of mechanical causes, the cause must logically be eliminated in order to treat the hemolysis. In the case of hemolysis to which a heart valve prosthesis is subject, in the worst case scenario it may become necessary to replace the prosthesis. Blood transfusions are often unsuitable for treating hemolysis.
prevention
One Hemolysis prevention is difficult and only under certain circumstances, such as the fact that hemolysis is not based on a genetic predisposition. Low-risk behavior, such as protection against possible intoxication or an autoimmune disease, are often the only ways to protect yourself from hemolysis.
Aftercare
In the follow-up and recovery phase of hemolysis, a transfusion can be initiated to deliver red cell concentrates to the patient. Doctors use it to alleviate the disease. If there are genetic causes, doctors often opt for surgical removal of the spleen, as treatment with drugs does not give satisfactory results.
In the subsequent phase, patients can change their lifestyle to minimize the risk of intoxication. A healthy lifestyle is an effective way to strengthen the immune system and reduce the risk of autoimmune diseases. This improves protection against hemolysis.
Patients should also look out for discoloration in the urine, which could indicate the disease. In the event of abnormalities, a short-term doctor's appointment must be made. The subsequent diagnosis shows whether the change is related to the disease. Those affected can protect themselves from the symptoms through a balanced diet and lifestyle.
Risk patients should avoid alcohol and stimulants such as coffee and nicotine, otherwise their general condition will deteriorate. Depending on the situation and fitness status, a gentle to moderate exercise program is advisable, which stimulates the circulation, stabilizes the immune system and reduces excess weight.
You can do that yourself
Hemolysis is a serious blood disorder that the patient can neither diagnose nor treat himself. It is often noticeable as a dark discoloration of the urine. However, there can be other causes for the discoloration of the urine. If the patient observes such a discoloration, he should immediately consult his doctor and have an appropriate diagnosis carried out. Side effects of hemolysis are a feeling of fatigue and exhaustion as well as sometimes severe headaches, which are caused by the disturbed metabolism.
The treatment of hemolysis is carried out in consultation with the doctor and under regular controls. It is very important that the patient adheres to the treatment plan discussed and shows up for the examinations. To support the treatment, the patient should refrain from all things and habits that put stress on the organism and thus weaken it.
Ideally, the patient will strive for a healthy and balanced lifestyle during hemolysis treatment. Consumption poisons such as alcohol, coffee in large quantities, nicotine or drugs should be avoided as a matter of urgency. Depending on the general condition of the patient, a light to moderate exercise or exercise program can strengthen the immune system and the cardiovascular system. This supports the organism in recovery. Obesity should be reduced.

.jpg)



.jpg)



.jpg)


.jpg)






.jpg)
