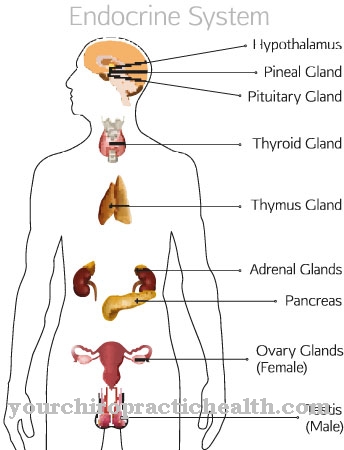
The testes migrate into the scrotum from kidney level during embryonic development. If this trek is not completed before birth, it is of one Testicular dystopia the speech. Testicular dystopias can now be treated surgically or with hormones.
What is testicular dystopia?

© Henrie - stock.adobe.com
Testicular dystopias are positional abnormalities of the testicle. The testicle lies temporarily or permanently outside the scrotum. The testicular dystopia corresponds to either a testicular ectopia or an undescended testicle. An undescended testicle is an incomplete descent of the testicle. That is, the testicle did not fully descend from the place of formation to its destination. This phenomenon is further differentiated according to the end of migration.
In addition to the pendulum testicle, the inguinal testicle and the sliding testicle, the one also counts Cryptorchidism about this phenomenon. In the testicle, the testicle has left the predetermined path on its migration from the place of formation to the place of destination. Depending on the ultimate location of the testicle, there are penile, femoral, transverse and perineal testicular ectomy. About three to six percent of newborns suffer from testicular dystopia.
causes
The testes arise at the level of the kidneys. A common gonadal system is their place of origin. Therefore, the testes must migrate down through the inguinal canal to the scrotal compartment. They move in the peritoneum along finger-shaped protuberances. This hike is also known as testicular descent. The descent of the testicles begins around the fifth week of pregnancy. The descent is only completed in the seventh month.
As soon as both testicles have reached their destination, there is a sign of maturity. A premature birth before the seventh month can interrupt the descent of the testicles. In this case, undescended testicles are only an expression of immaturity and can regress by the actual due date. Another cause can be the use of analgesics during pregnancy.
Disorders in the hormonal cycle, genetic causes or anatomical obstacles can also be considered as causes for permanent undescended testicles.
Symptoms, ailments & signs
In the undescended testicle, the testicle may have migrated on the intended path, but its migration has come to an early halt. The signs of undescended testicles differ with the type of abnormality. In cryptochism, for example, the testicle is located in the abdomen. The inguinal testicle corresponds to a testicle that has remained in the inguinal canal.
The sliding ode has almost reached its destination, but because of a short spermatic cord it lies in the inguinal canal, from where it can be pushed into the scrotum. The pendulum testicle has reached the scrotum, but moves out of the scrotum when excited. In contrast to undescended testicles, during a testicular ectomy the testicle has left the intended path during its migration.
The femoral testicle means a testicle under the skin of the thigh. The perineal testicle lies in the perineal area, the penile testicle is shifted to the penile shaft and the transverse testicle lies in the scortal compartment on the other side.
Diagnosis & course of disease
The diagnosis of testicular dytopia can be made using various examinations. One of the most important examinations is palpation. Under certain circumstances, a laparoscopy or an ultrasound examination can also be useful. Not all testicular dystopias are at the same risk or require treatment at all.
A pendulum testicle, for example, carries little risk, while other testicular dystopias are associated with a certain risk of degeneration. Without adequate therapy, the risk of developing a malignant testicular tumor for those affected can be up to 32 times higher. Testicles that remain in the abdomen, for example, harbor the highest risk of degeneration. Testicular dystopia can also endanger fertility. Anomalies in the position of the testicles are one of the most important causes of impaired fertility.
Complications
Testicular dystopia causes the testicles to be incorrectly positioned in the body of the born child. As a rule, the position cannot be predicted because the severity of the symptom can vary. After the birth, however, surgical interventions can be undertaken to correct the symptoms. In most cases, there are no particular complaints or complications.
Due to the migration of the testicles, the patient usually does not experience any particular symptoms. However, the risk of developing a tumor increases extremely, so that treatment is highly recommended and in most cases is carried out. Furthermore, testicular dystopia can also lead to infertility and thus extremely limit the life of the person affected in adulthood.
This can lead to various psychological complaints and complications, so that those affected often suffer from depression and reduced self-esteem. The partner can also develop depressive moods. In most cases, the treatment takes place after the birth and does not lead to complications. In some cases, the testicular dystopia disappears on its own, which is why the doctor usually waits six months after the birth before the operation.
When should you go to the doctor?
Testicular dystopia is usually diagnosed by the responsible doctor or obstetrician immediately after the birth. Treatment is required if the undescended testicle does not resolve on its own within a few hours to days. Parents who experience pain or other discomfort in their child should speak to their doctor. If complications such as severe pain or circulatory problems develop in the scrotum area, the child must be treated in a hospital.
Testicular dystopia always requires clarification by a pediatrician or a urologist. Otherwise, the misalignment can lead to infertility and testicular cancer. People diagnosed with testicular dystopia in childhood should have regular urological examinations in adulthood. Close monitoring ensures that no new incorrect position develops. If there are already signs of infertility or any other illness, the patient must be examined for possible undescended testicles and treated if necessary.
Doctors & therapists in your area
Treatment & Therapy
As a rule, no therapeutic steps are initiated in the first six months after the birth. During this time, the doctors wait to see whether the testicle might still move into the intended position. If the testicle does not move into its position on its own, the descent can be promoted by giving hormones. For four weeks, those affected are given gonadoliberin as part of hormone therapy.
This is followed by a three-week treatment with β-hCG. Both hormones are usually given to the infant in the form of a nasal spray. In about 30 percent of the cases, this treatment leads to the goal. If the hormonal treatment is not effective, the testicle is surgically fixed in the scrotum between the 9th and 18th month of life. This surgical correction is also known as orchidopexy. The testicle is fixed at the lowest point of the scrotum in order to prevent further rotation out of the scrotum.
The mobility of the testicle is restricted by sutures. The procedure is performed under general anesthesia. In the first step, the surgeon exposes the testicle and in the second step brings it into position, where he sutures it to the layers of skin on the scrotum. After the operation, regular check-ups are indicated to rule out recurrences. Repeated hormone therapy is sometimes recommended after an operation.
You can find your medication here
➔ Medicines for painOutlook & forecast
The prognosis of testicular dystopia is to be classified as favorable. With today's medical options and different therapeutic approaches, treatment takes place within the patient's first years of life. The anomaly of the testicle is determined immediately after birth in the routine postnatal examinations and diagnosed later by means of imaging tests.
If the testicular dystopia does not heal spontaneously, the baby is treated with medication after the first six months of life. A deterioration in the state of health is not to be expected within the first months of life. Usually the state remains unchanged. Rather, the organism is given sufficient time so that an independent and naturally initiated correction of the testicle positioning can take place.
If this does not take place, external options are used. The administration of hormonal preparations already corrects and thus heals testicular dystopia in many patients. In most cases this leads to lifelong freedom from symptoms. If the hormone therapy remains ineffective or does not show the desired success, a correction is made in a surgical procedure. If no further complications arise during or after the operation, the patient is discharged from the treatment as cured. After a while, a check-up follows so that a relapse can be excluded.
prevention
The cause of testicular dystopia has not yet been conclusively clarified. Since analgesics are causally relevant, not using them during pregnancy can prevent testicular dystopia if this is possible for health reasons.
Aftercare
The treatment of testicular dystopia should be completed when the child is one year old. Any subsequent relocation of the testicles back into the scrotum carries a higher risk of fertility. If surgery was performed as therapy, direct follow-up care in the clinic is initially the responsibility of the doctors.
After discharge, the parents must first ensure bed rest and restrain the child in his play behavior in the first week in order to prevent complications and a new undescended testicle. After its operative relocation, the testicle must first fused in its new position in the testicle in order to be permanently fixed. Up to this point in time, a careless movement, despite the presence of an internal seam, can lead to a shift back.
After about seven to ten days, the first follow-up examination takes place to check the position of the testicles and the wound healing that has taken place so far. The attending physician can assess whether the restricted mobility can already be relaxed or whether it must be maintained for a further six weeks until the next examination. From now on, quarterly follow-up checks will be carried out on average up to the end of a year.
The possibility of a developing testicular tumor persists into adulthood despite surgery and therefore requires visits to the urologist until after puberty. In the event of enlargement or hardening of the testicle, the attending physician should be consulted immediately.
You can do that yourself
Parents who notice signs of testicular dystopia in their child should contact their pediatrician immediately. In some cases, the testicle will move back into place on its own and no further treatment is necessary.
If drug or surgical treatment is necessary, care must be taken that the child is not exposed to any additional stress and that it is as gentle as possible. Physical exercise should only take place to a limited extent in the first few days so that the testicles can move back into their position or remain in the scrotum after an operation. If you are in pain, your doctor may prescribe a mild medicine. Medicines from naturopathy, for example marigold ointment or preparations with arnica, may also be allowed.
After an operation, the scrotum should be cooled slightly so that the swelling disappears quickly. Strict hygiene measures can prevent complications such as wound healing disorders or infections. In addition, medical monitoring of the testicles is required. Sometimes testicular dystopia occurs again, which must be recognized as quickly as possible and treated accordingly. It is believed that testicular dystopia can be avoided by avoiding analgesics during pregnancy.



.jpg)


















.jpg)

.jpg)
