At a hypovolemic shock there is a severe circulatory disorder which, if left untreated, leads to death. The cause is usually a loss of blood or fluid, for example due to severe diarrhea or bleeding after an accident.
What is Hypovolemic Shock?

© peterschreiber.media– stock.adobe.com
In colloquial language one often speaks of shock as a result of a situation with extreme psychological stress. In medicine, the term denotes hypovolemic shock however, an acute lack of oxygen in vital organs such as the lungs or kidneys. The relationship between oxygen demand and the supply of oxygen is no longer correct.
A lack of volume leads to a centralization of the remaining blood volume and thus to a reduced perfusion of the smallest blood vessels (capillaries). Due to the lack of blood flow, there is a lack of oxygen and damage to the cells and thus to the entire organ. This can lead to a loss of function of the affected structures.
causes
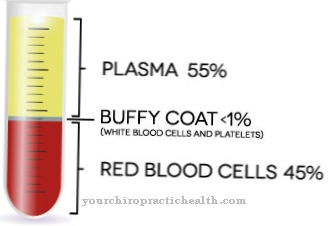
The cause of hypovolemic shock is a lack of volume. It occurs when more than 20 to 30 percent of the total blood volume is lost and other fluid losses. Hypovolemic shock, caused by loss of blood, is also called a hemorrhagic shock.
Injuries to vessels, for example through cuts or the rupture of an aneurysm, i.e. a vascular sac in the main artery, can result in massive blood loss and thus cause hypovolemic shock. Bleeding in the gastrointestinal tract, for example from stomach ulcers or tumors in the intestine, can be so massive that the blood volume is no longer sufficient to completely supply the body.
Another source of heavy bleeding is acute, severe inflammation of the pancreas (pancreatitis). Other causes of profuse bleeding that can trigger hypovolemic shock include fractures in bones with good blood supply, such as a fractured pelvis or thigh. The rupture of the spleen, for example after an accident or accidental injuries to other organs, can lead to bleeding into the abdominal cavity and thus to a loss of volume that cannot be compensated for.
Complications during childbirth or during operations also carry the risk of life-threatening blood loss. Not only the loss of blood, but also the loss of water, plasma or electrolytes can lead to volume depletion shock. Possible causes here are losses due to severe vomiting, diarrhea, dehydration due to insufficient fluid intake or disorders in the hormonal balance with increased water loss (for example adrenal insufficiency Addison's disease).
In the case of severe inflammation of the peritoneum or lungs, as well as extensive burns, the loss of plasma water into the tissue can be so severe that hypovolemic shock develops.
Symptoms, ailments & signs
If there is a reduction in blood volume due to blood or fluid loss, the body first tries to stabilize the circulation by increasing the cardiac output. In addition, adrenaline and noradrenaline are released in order to constrict the blood vessels. The heart also beats faster because of the adrenaline. These measures result in a redistribution of the residual blood.
The blood is withdrawn from organs and body structures that are not directly vital, such as the skin, arms and legs, the gastrointestinal tract and the kidneys, in order to be able to supply the indirectly vital organs such as the brain, heart and lungs. This process is called circulatory centralization.
Patients in shock or on the verge of shock are usually very restless and anxious. The release of adrenaline and noradrenaline increases the pulse rate to more than 100 beats per minute. The patients get cold sweats. The blood pressure is low due to the low blood volume and systolic is below 90mmHg. If circulatory centralization has already taken place, the pulses in the body periphery, for example on the wrist or foot, can no longer be felt.
Due to the reduced blood flow to the skin, those affected are pale gray and feel cold. The skin and mucous membranes are colored blue (cyanotic) due to the lack of oxygen. The urine excretion is limited or completely stopped due to the functional impairment of the kidneys. There is difficulty breathing or hyperventilation. A strong feeling of thirst is also typical of hypovolemic shock.
Diagnosis & course of disease
The diagnosis of hypovolemic shock is usually based on the typical clinical picture paired with the symptoms of the possible cause. The shock index can be used to assess the dangerousness of the situation. The shock index is the quotient of pulse rate and systolic blood pressure. In healthy people this index is approx. 0.5, in shock the value rises to over 1, which means that the pulse is higher than the systolic blood pressure.
The Rekap test is used to diagnose the peripheral blood flow situation. The examiner briefly presses the nail of the affected person into the nail bed. This will force the blood out of the capillaries. If the re-capillarization, i.e. the backflow of blood into the capillaries, lasts longer than a second, it is assumed that there is insufficient blood flow in the periphery.
Complications
If the shock is not treated by a doctor, the patient usually dies. For this reason, immediate treatment is necessary to keep the patient alive. There is a severe loss of blood and fluid. If these losses persist and are not stopped immediately, the internal organs and heart can no longer function.
Furthermore, the organs are supplied with too little oxygen, so that consequential damage can occur, which is usually irreversible. Due to the low blood pressure, the patient loses consciousness and can suffer various injuries from a fall. Shortness of breath occurs, which is usually accompanied by hyperventilation.
Treatment of shocks is symptomatic and primarily stops bleeding and fluid loss. If this is done quickly enough, the sufferer can survive. However, it cannot be predicted whether the shock caused irreversible damage to the organs or the brain. This can lead to paralysis or other sensory disorders, for example. Life expectancy can also be limited by the shock.
When should you go to the doctor?
In the event of hypovolemic shock, an emergency doctor must be alerted immediately. The patient needs intensive medical treatment immediately. If the blood pressure suddenly drops and there is shortness of breath, the emergency services must be called. A strong feeling of thirst is also typical of the shock reaction, which cannot be eliminated by ingesting fluids. If symptoms are noticed, it may be caused by hypovolemic shock and require medical evaluation and treatment. If you have severe cuts or signs of an aneurysm, you must see a doctor immediately.
People who suffer from stomach ulcers or tumors in the intestines also belong to the risk groups. Patients who suffer from inflammation of the pancreas should speak to their doctor if they have symptoms mentioned. In the event of hypovolemic shock, emergency medical help is always required. Other contacts are the family doctor or an internist. People who experience a shock reaction in connection with an existing illness should speak to the responsible medical professional.
Doctors & therapists in your area
Therapy & Treatment
The most important therapy for volume depletion shock is the rapid replacement of fluid. This is usually done by supplying isotonic infusion solutions. In the case of hypovolemic shock caused by blood loss, stopping the bleeding is of course in the foreground of the treatment. In addition, possibly damaged organs must be treated.
The occurrence of a shock kidney, i.e. kidney failure in shock, must be prevented in any case. The same goes for the shock lung. The shock position is recommended as the first measure in hypovolemic shock. Here, the patient is laid down and the legs are raised. This leads to a backflow of blood from the legs and thus to a larger volume of blood in the upper body.
prevention
To prevent hypovolemic shock, care should always be taken to ensure adequate fluid intake in the event of severe infections, diarrhea or vomiting. Obvious bleeding should be stopped as soon as possible. In any case, the emergency doctor should be notified directly even if there is a mere suspicion of a volume deficiency shock.
Aftercare
After the primary measures in hypovolemic shock, the aim is to return to normal. For this purpose, the patients receive red cell concentrates and, depending on the situation, fresh plasma. Volume substitution also supports the recovery of the affected person. For further follow-up treatment it is important that an intensive discussion takes place between the doctor and the patient.
In this way, the endangered person learns worth knowing details that relate, for example, to the correct behavior in a state of shock. If family members and acquaintances are informed accordingly, worse consequences can be avoided. For good blood circulation in the upper body, the patient's legs should be a little higher.
Special precautionary measures must be taken, especially in the event of an infection that is accompanied by nausea. Adequate fluid intake plays a vital role here. In the case of open bleeding, increased attention is also required. A precise line between first aid, aftercare and prophylaxis cannot be drawn here.
People with a corresponding indication should learn to be aware of their own body so that they can react quickly to any warning signs. In close cooperation with the doctor, other complaints such as kidney failure can also be avoided. If there is trauma related to the shock, therapeutic assistance may also be needed.
You can do that yourself
If hypovolemic shock occurs, the emergency doctor must be alerted immediately. The cause of the shock must then be determined and, if possible, eliminated, for example by stopping bleeding or immobilizing a broken bone. The patient must be reassured and should, if possible, go into the shock position - legs about 20 to 30 degrees higher than the rest of the body. The ambulance service will provide oxygen to the injured person and take him to a hospital for further treatment.
The further self-help measures are based on the injury. In the case of broken bones and similar injuries, rest is indicated first and foremost. The wound should be cared for according to the doctor's instructions in order to avoid wound healing disorders and other complications. At the same time, the injury must be regularly examined by the responsible doctor. Sometimes the patient also needs therapeutic help to cope with trauma. The further steps depend on the physical and mental condition of the person affected and the healing process of the offending injury.

.jpg)