The Jugular vein thrombosis is the formation of a blood clot in the neck or jugular veins. The formation of a thrombus does not have to be associated with coagulation disorders, but can refer to malignant diseases or be a sign of a bacterial infection. The administration of heparin prevents the thrombus from further growth.
What is jugular vein thrombosis?

© Sebastian Kaulitzki - stock.adobe.com
Thromboses are vascular diseases. A blood clot or thrombus forms in the blood vessels. Thromboses can affect all blood vessels. Veins are most commonly affected by thrombus formation. In this case, we are also talking about venous thrombosis or phlebothrombosis.
The Jugular vein thrombosis affects the jugular veins, also known as the internal, external, and anterior jugular veins. These vessels are located in the head and neck area and emerge from the structure of the cranial cavity through the posterior part of the jugular foramen. In jugular vein thrombosis, there is usually a unilateral thrombotic occlusion of the large jugular veins. The internal jugular vein is most commonly affected.
The occlusive disease occurs comparatively rarely in the jugular veins and is characterized by an extremely variable clinical course. The phenomenon used to have a high risk of sepsis. Nowadays, a septic course is rather the exception. Bacterial inflammation has not been a common cause of jugular vein thrombosis since the introduction of the antibiotic.
causes
The jugular vein thrombosis can be a complication of therapeutic interventions and often occurs, for example, with the insertion of a central venous catheter or extensive interventions in the neck area. In addition, masses such as tumors can obstruct the vein and thus promote the formation of a thrombus.
Cervical inflammatory processes caused by neck phlegmons, in the context of a peritonsillar abscess or as a result of mastoiditis can also cause jugular vein thromboses. More rarely, thrombosis is the result of intravenous drug abuse with injections into the neck veins. Causes such as blunt neck trauma or general clotting disorders are far more common. Jugular vein thrombosis can also occur as a secondary phenomenon in the context of pancreatic cancer, bronchial cancer, gastric cancer or ovarian cancer.
Symptoms, ailments & signs
The clinical picture of jugular vein thrombosis is variable. Some patients develop a feverish course. They complain on one side of painful swellings in the neck, which move them to relieve themselves. This relieving posture can lead to tension and pain in the cervical spine.
In some cases, the thrombosis also causes swallowing and voice disorders by pressing on the vocal cords, windpipe, or esophagus. Some patients are sensitive to pressure in the area of the vascular cord. Sepsis following the thrombosis can occur in the context of bacterial infectious thrombi, but is rather rare today.
Unspecific symptoms such as swelling of the neck, headache or enlarged cervical lymph nodes are more common accompanying symptoms. A coarse, consistent cord may be palpable in the course of the affected vein. In some cases the Queckenstedt mark is positive. In exceptional cases, jugular vein thrombosis does not cause any symptoms.
Diagnosis & course of disease
In asymptomatic patients, jugular vein thrombosis is usually discovered as an incidental finding during sonographic examinations. Sonography is always the method of choice for diagnosis. Imaging procedures such as CT or MRT can also allow a reliable diagnosis, but they put a strain on the patient with contrast media.
Therefore, if a thrombosis of the neck veins is suspected, sonography should be given priority. In laboratory tests, patients can show an increase in D-dimers. In the case of infections, there are increased infection parameters such as the C-reactive protein or leukocytosis. To differentiate the thrombosis from a degeneration of the lymph nodes.
Malignant lymph nodes resemble a thrombotic vein occlusion at first glance, especially in axial slices, and must be clearly ruled out if the findings are appropriate. The prognosis of the patient depends on the primary cause of the thrombosis.
Complications
Jugular vein thrombosis can lead to various complaints and restrictions in the everyday life of the person affected. In most cases, however, patients have a severe fever and a general feeling of illness. In addition, there is often a feeling of exhaustion and the resilience of the person concerned is significantly reduced and restricted by the jugular vein thrombosis.
Furthermore, there is severe swelling in the neck area. The neck appears tense and pain occurs in these regions. It is not uncommon for the pain to spread from the neck area to other regions of the body and can also lead to discomfort there. This leads to headaches and, in the case of resting pain, continued sleep disorders.
The patient's quality of life is severely limited and reduced by the symptoms of jugular vein thrombosis. A sore throat can also occur. Treatment of jugular vein thrombosis can be done with the help of medication and, as a rule, leads to a positive course of the disease. There are no particular complications. In most cases, this disease does not reduce life expectancy either. The affected person may be dependent on the intake of blood thinners.
When should you go to the doctor?
Swelling on the neck is an indication of irregularities that should be examined by a doctor. If the symptoms persist or if they increase in intensity, a doctor should be consulted as soon as possible. Particular attention should be paid to the changes on the neck, in the absence of any colds. If irregularities can be felt externally, they should be presented to a doctor. Since jugular vein thrombosis, if left untreated, can lead to premature death, a medical examination is necessary in good time to clarify the cause.
Tensions in the cervical vertebrae that set in without a bad posture are considered unusual. It is recommended to have it assessed by a doctor. If there is pain in the neck area or if the head and neck are relieved, these are warnings that should be followed up. In the case of speech disorders, impaired breathing or peculiarities during the swallowing process, a visit to a doctor is advisable.
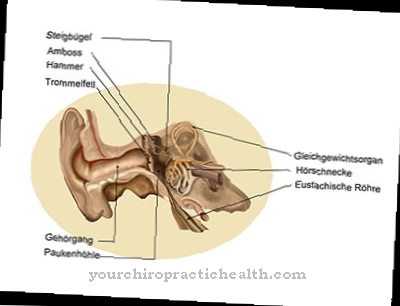
If food intake is refused due to swallowing difficulties or if the fluid intake is reduced, the organism may be under-supplied in the further course of the process. A doctor visit is required as soon as a feeling of internal dryness sets in or there is severe weight loss. Otherwise, dehydration threatens a life-threatening condition. Lymph swelling, dull hearing, or headache should also be fully evaluated by a doctor.
Treatment & Therapy
Basically, the treatment of a jugular vein thrombosis always depends on the underlying disease or the cause of the thrombus formation. The causal therapeutic administration of heparin is always indicated in the case of excessive blood coagulation. In order to rule out complications such as sepsis in the case of a bacterially infectious cause, certain antibiotics are administered depending on the respective pathogen.
Intraluminal lysis therapies are usually not carried out, as they increase the risk of sepsis. If sepsis is imminent or has already started, this phenomenon is the main focus of treatment. In extreme cases, sepsis may require surgically invasive ligature or even partial or full resection of the affected vein. In the case of causal coagulation disorders, the treatment of thrombosis is usually much easier with the administration of anticoagulant heparin preparations.
Once the thrombus has stopped growing, the body can start cleaning up and breaking down the clot. Artificially induced thrombolysis has not been used in most cases recently to dissolve thrombi in the area of the veins.The reason for this is the risk of bleeding that arises during thrombolysis within the veins.
Outlook & forecast
Jugular vein thrombosis takes an unfavorable course without medical treatment. This disorder causes blood clots to form around the neck and head. If the person concerned does not seek medical care or medical care, the thrombus can be expected to grow. As a result, existing complaints gradually increase in intensity and over time new irregularities appear, which lead to a decrease in well-being. In addition to headaches, swallowing disorders and swelling, there is a general decrease in quality of life. Daily responsibilities become increasingly difficult and complications can arise.
When seeking medical care, the thrombus is removed in one procedure. This is associated with the usual risks and side effects. If the procedure goes without further complications, the blood circulation is regulated and the health impairments are alleviated. In many patients, freedom from symptoms can be documented a short time after the thrombus has been removed.
Although recovery has been achieved, there is still a chance that this condition will recur. A relapse in the course of life is possible at any time. The prognosis is unchanged if the jugular vein thrombosis is repeated. The sooner the disease is diagnosed and treated, the better and faster the symptoms can be alleviated.
prevention
Especially patients with increased blood clotting due to blood that is too thick can prevent the formation of thrombi by taking certain medications on a long-term basis. Blood-thinning drugs based on acetylsalicylic acid or ASA are sometimes used for this.
There are also various home remedies for blood thinning, such as ginger, nuts, avocado and pomegranate. The use of home remedies in no way replaces medical advice or medical drug care, but should, if indicated, be used in combination with the drug intake.
Aftercare
The measures of direct follow-up care are in most cases severely limited in jugular vein thrombosis. The person affected should ideally contact a doctor at an early stage so that no further complications or complaints arise for the person concerned, as this disease cannot heal independently. The earlier a doctor is consulted, the better the further course of the jugular vein thrombosis is usually.
Treatment for this disease is most often done by taking various medications. In any case, the person affected should ensure that they take the medication regularly and that the dosage is correct in order to permanently alleviate the symptoms. If anything is unclear or if you have any questions, a doctor should always be consulted first. Regular checkups by a doctor are also very important for this disease.
A doctor should be consulted in the event of severe bleeding or injury. In many cases, patients with this disease are dependent on the help and support of their own family or friends. Loving and intensive conversations are also useful, as this can also prevent psychological complaints or depression.
You can do that yourself
In most cases the patient with a jugular vein thrombosis has no means of self-help. In any case, medical treatment is necessary for this disease to prevent further complications.
Since the person concerned is often dependent on the intake of antibiotics with this disease, possible interactions with other drugs should be considered. It is best to tell the doctor about other medications you are taking to avoid these interactions. You should also strictly refrain from consuming alcohol when taking antibiotics.
In order to avoid the formation of thrombi in general, the person affected should take blood-thinning medication if they have known previous illnesses. There are also various foods available to those affected, such as avocado, ginger, nuts or pomegranate. Nevertheless, those affected depend on the ingestion of heparin to prevent blood clotting. Contact with other affected persons often also helps, as this leads to an exchange of information that can make the patient's everyday life easier. If there are psychological complaints, it is very helpful to talk to your own friends or relatives.



.jpg)