The juvenile xanthogranuloma Mostly affects children under one year of age and often resolves or fades on its own. It is a yellow-orange spot or a benign hemispherical tumor. As long as it is not located in the eye, the xanthogranuloma only needs medical treatment in very rare cases.
What is juvenile xanthogranuloma?

© Monkey Business - stock.adobe.com
A juvenile xanthogranuloma (JXG) is a benign, non-Langerhans cell histiocytosis that occurs predominantly in infants and young children under two years of age. It is a collection of lipid-laden macrophages. Even at birth, smooth, dome-shaped nodules and papules with the typical yellow-orange color can appear.
It most commonly occurs around the age of 2. Less common in older children and even less common in adults. Benign means benign and not aggressive. In individual cases, other organs can be involved. These include eyes, spleen, liver, lungs, and the central nervous system, but this is comparatively rare. The juvenile xanthogranuloma is also called Non-X histiocytosis, Xanthogranuloma juvenile or Nevoxanthoid endothelioma designated.
causes
Nothing is known exactly about the causes of xanthogranulomas. It is possible that genetic dispositions are behind the development of these skin changes. In any case, it is an overproduction of histiocytes and dendritic cells, which accumulate and lead to different symptoms depending on the location.
Symptoms, ailments & signs
The JXG is mostly characterized by solitary yellow-orange nodules or raised papules 0.5 to 2 centimeters in diameter. These can also appear reddish at the beginning. They are mainly visible in the head area, on the neck or upper body and on the extensor sides of the extremities and are relatively harmless.
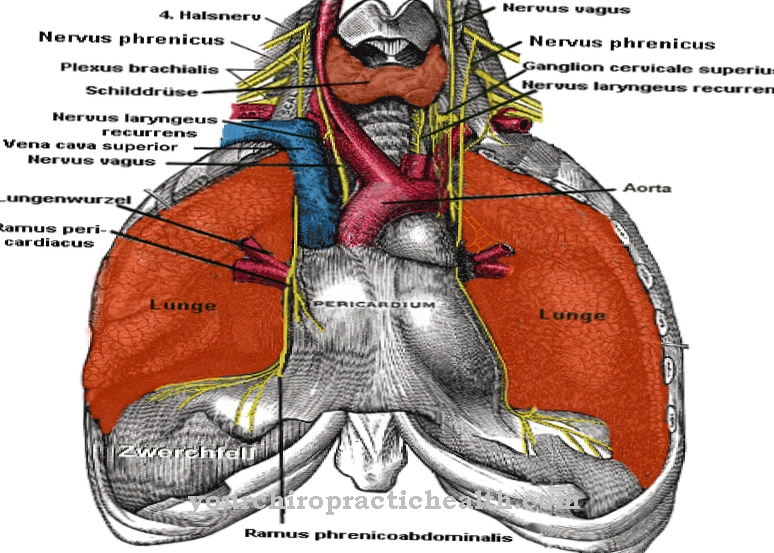
However, if they occur on or near the eyes and possibly even multiple, i.e. multiple times, an ophthalmologist should be consulted. With an ophthalmological examination, a risk to the eyesight must be clarified. In rare cases, the juvenile xanthogranuloma can lodge in other organs. There are a number of options for this. In addition to the above, they have also been observed in the kidneys, bones, muscle tissue, adrenal glands, the testes (testicles) in the larynx (windpipe), in the intestines and in the pericardium (heart muscle).
Diagnosis & course of disease
A visual diagnosis is often enough to identify the characteristic skin signs. Modern examination equipment and high-resolution microscopes enable younger patients to use diagnostic methods that are gentler than a few years ago. Infants who are affected during birth and up to the first six months of life are more likely to have multiple lesions.
A fall frequency of ten percent of births is assumed and it is noteworthy that male babies are more frequently affected. In unclear cases, Langerhans histiocytosis, neurofibromatosis type 1 and juvenile myelomonocyte leukemia must be excluded. These are the most common dangerous diseases that the JXG can be confused with.
Other differential diagnoses are: Molluscum contagiosum, Feuerstein-Mims-Schimmelpenning-Syndrome, Keloid scar, urticaria pigmentosa, histiocytoma, fibromatosis, digital, infantile, Spitz nevus, fibroma, xanthoma tuberosum and eruptivum. Normally, no tissue samples are taken from infants and toddlers unless absolutely necessary, because juvenile xanthogranuloma usually disappears on its own by the age of six.
The most common place of extracutaneous occurrence is in the eyes with the eyelid and iris. About half of these small patients have skin lesions, making juvenile xanthogranulomatosis the most common cause of spontaneous hyphema in the iris and ciliary body.
This means an accumulation of red blood cells in the anterior eye area, as occurs in blunt trauma, for example in boxing. In the affected children, this leads to secondary glaucoma and, subsequently, often even to blindness. The treatment is therefore a great challenge for every ophthalmologist.
If the disease occurs in adults, the diagnosis is difficult and a high number of unreported cases is assumed. In addition, spontaneous healing no longer occurs, as with most children. Depending on the location, the most varied of symptoms occur, which can also be assigned to numerous other diseases. Therefore, these diagnoses are possibly more incidental findings when diagnosing other diseases.
Complications
In most cases, this condition does not require any special treatment. In most cases, the stain or benign tumor will go away on its own, so there are no further complications or symptoms. As a rule, a small lump is visible in the child. However, if the disease is directly on the eye or in the vicinity of the eye, an ophthalmologist must be consulted.
In this case, the lump can affect the patient's eyesight and thus reduce the patient's quality of life. The disease can also occur in other internal organs and lead to complaints or complications there as well. The further course mostly depends on the affected region of the patient. In most cases, treatment for this disease is not necessary.
The symptoms usually go away on their own without any particular complications. This does not limit the patient's life expectancy. Furthermore, the tumor can also be limited by radiation or chemotherapy. There are usually no further complications.In some cases, psychological support for the parents or relatives is also necessary.
When should you go to the doctor?
Usually, juvenile xanthogranuloma does not require a doctor's visit. The skin abnormalities appear in newborns and infants. Spontaneous healing occurs within a few weeks or months without any further sequelae. A doctor's visit can be made to protect and reassure the parents. Often, however, the information from the obstetrician is sufficient through visual contact. Since routine check-ups of the newborn are carried out within the first months of life, the skin changes are usually addressed and clarified by a doctor during these treatment appointments.
In rare cases, the granuloma develops in parts of the body that require medical intervention. If the changes in the complexion of the skin develop in the vicinity of the eye, this can lead to impaired vision. If discoloration of the skin or new tissue formation in the form of poplars is observed in the region around the eyelids, a doctor should be consulted. Medical treatment is advisable if the eyesight is at risk. In exceptional cases, the granulomas can attach to various organs inside the body.
A doctor should therefore be consulted in the event of abnormal digestion or a decrease in the infant's appetite. If there is significant weight loss, diarrhea, constipation or pain in the abdomen and kidney region, a doctor is recommended.
Treatment & Therapy
There is no special therapy for infants and young children and it is usually not appropriate, as juvenile xanthogranulomas often go away on their own. However, if they are close to the eyes, very low-dose radiation can be used to contain the growth.
There are various options for extracutaneous JXG, depending on the location. Chemotherapy similar to therapy for histiocytosis X can be used for larger accumulations in the abdomen and organs, as well as in the nervous system. The extracutaneous JXG is one of the rare diseases for which hardly any research funds are made available. Therefore, there is still no standard therapy for this that can be used in individual cases.
You can find your medication here
➔ Medicines for painOutlook & forecast
Juvenile xanthogranuloma has a favorable prognosis in almost all patients. In most cases there is spontaneous healing. The changes in the appearance of the skin do not pose a further threat to the health of the person concerned. Treatment or the intervention of a doctor is only rarely necessary. The granulomas occur primarily in children and disappear within a few days, weeks or months.
If the skin changes have not been scratched up and open wounds have developed, they have no disease value. If there are open wounds, there is a risk of blood poisoning. The wounds can contaminate and germs can get into the organism via the entry points. A worsening of the prognosis is to be expected, as sepsis is potentially fatal. In addition, secondary diseases can arise.
If granulomas develop near the eye, the otherwise favorable prognosis also deteriorates. At this point on the body, they can lead to impaired vision. Medical care is necessary to avoid complications and to remove the lesions. If the treatment proceeds without further incidents, the patient can also be discharged from the treatment within a short time as recovered. A relapse is possible in the further course, especially during childhood. The favorable prognosis remains in these cases.
prevention
Juvenile xanthogranuloma cannot be prevented and the mechanisms of action and how it occurs have not yet been fully understood. The Histiocytosis Association is working closely with an international group of physicians to advance research in this area and to give these rare patients a chance of a cure in the future.
Aftercare
In many cases, there are no special follow-up measures available to those affected with this disease. First and foremost, a very quick diagnosis and subsequent treatment are important so that there are no further complications in the life of the person concerned. In some cases, this tumor can resolve on its own, but the disease should still be checked by a doctor.
If the disease goes away on its own, no special follow-up care is necessary or possible. Those affected should, however, regularly undergo various examinations and checks by a doctor in order to identify and treat other tumors or other complaints at an early stage. Since the disease occurs primarily in children, they must be supported accordingly by their parents and other relatives.
Intensive and loving discussions are also very important here, as this primarily prevents depression and other psychological upsets. Parents should also take care that children do not scratch the changes on the skin. Only in a few cases does this disease limit the life expectancy of the person affected.
You can do that yourself
For patients with juvenile xanthogranuloma, it is of the utmost importance to carefully observe the changes associated with the disease and to visit the treating doctor immediately if the granuloma is enlarged or otherwise. It is also advisable that the parents take the affected child to regular preventive check-ups in order to register changes in good time and initiate adequate therapy.
In many cases, juvenile xanthogranuloma disappears on its own in young people and does not require medical treatment. Then patients and guardians only support the course of the disease by taking care not to irritate the juvenile xanthogranuloma. Irritations are possible, for example, from cosmetics or injuries caused by rubbing clothes or hand movements during personal hygiene. Therefore, patients are particularly vigilant and careful during such activities so as not to provoke negative changes.
Treatment is necessary if the granuloma is close to the eye and threatens to impair visual function. In such cases, care by ophthalmologists and other specialists is required to remove the juvenile xanthogranuloma and thereby prevent complications in good time.

.jpg)