Cocci occur in several forms of organization and can lead to severe infections if they multiply and the infected person has a weakened immune system. Various cocci subspecies are so adaptable that they have already developed strains that are resistant to conventional antibiotics. It is particularly treacherous that cocci can repeatedly cause severe food poisoning despite good food hygiene.
What are cocci?
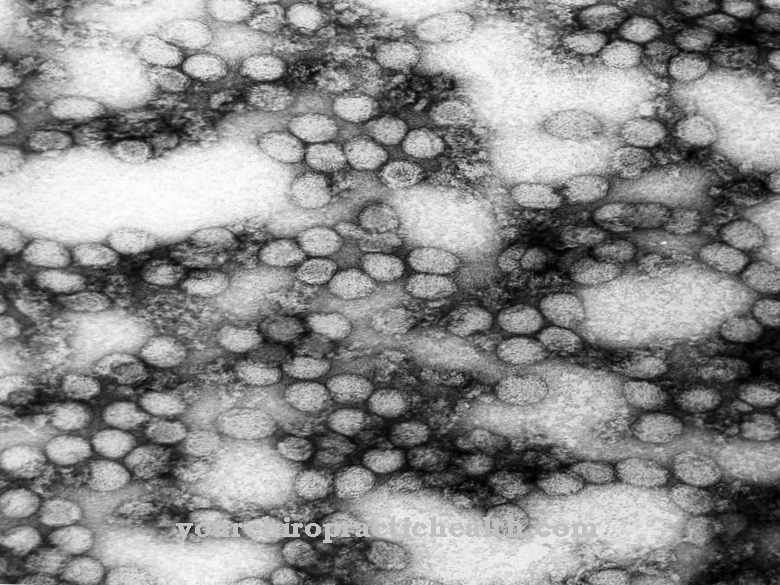
Cocci are spherical bacteria that are either completely round or ovoid or elliptical in shape. The medical layperson can recognize that certain types of bacteria are cocci by the name ending -coccus. Cocci come in different forms of organization, depending on the level of division at which they have not separated from each other. The most well-known representatives are staphylococci, streptococci and enterococci.
If the bacteria, which are normally found in every human being and animal, meet particularly favorable conditions and multiply quickly, they can cause dangerous diseases and even lead to death. Especially immunocompromised people, diabetics, neurodermatitis sufferers and hospitalized people (patients and hospital staff) are particularly at risk of contracting a cocci infection. Most cocci are treated with common antibiotics. However, there are now strains that are resistant to certain antibiotics.
The staphylococci were first described by Friedrich Julius Rosenbach in 1884. Enterococci used to be considered serogroup D streptococci because, like streptococci, they have the group D Lancefield antigen. However, since 1984 they have been regarded as an independent genus of cocci due to their different genetic structure. They belong to the lactobacilli (lactic acid bacteria).
Occurrence, Distribution & Properties
The spherical bacteria are organized in groups of two (diplococci), tetrads (groups of four), or as chain cocci, packet cocci (quadrangular agglomeration of 8 or more spherical bacteria) or cluster cocci (in the form of grapes). Staphylococci occur in clusters and colonize the surfaces of the skin and mucous membranes in large numbers - which is not a problem for people with an intact immune system.
The gram-positive pathogens have no movement of their own and feed on putrid substances (saprophagous). Because they have a high pH tolerance, some disinfectants cannot kill them. Dehydration cannot harm them either.
Since they can adapt quickly to new environments through mutation, they spread rapidly and can trigger epidemics. It is transmitted from person to person through direct contact with an infected person, through infected objects and food. The incubation period after infection with staphylococci is 4 to 10 days. Infected patients may not show symptoms until months later. In the case of food poisoning, the first signs of illness appear after a few hours.
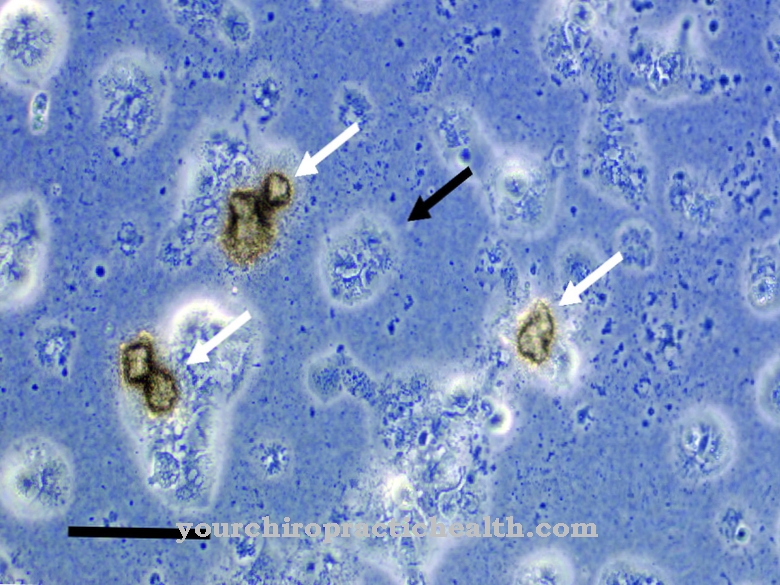
The most important representatives are Staphylococcus aureus, which colonizes the skin and mucous membranes, and Staphylococcus epidermidis, which lives on the skin and other surfaces and is feared in hospitals because of its resistance to penicillin and methicillin. It is transmitted there via infected devices, blood, cough secretions, wound secretions and skin contact. It enters the patient's body via transplanted heart valves, artificial joints and indwelling vein catheters.
Streptococci colonize the oral cavity and are usually harmless. The gram-positive spheroidal bacteria organize themselves individually or in pairs in more or less long chains. They cannot move on their own and do not form spores. Some trunks are surrounded by a sheath of mucus. They live anaerobically, but can be exposed to oxygen and are created through fermentation processes. Enterococci also form chains and are part of the normal intestinal flora in animals and humans. They are also found in foods such as cheese and sausage.
Illnesses & ailments
Staphylococcus aureus enters the bloodstream through wounds and injuries. Outwardly, it causes eczema, boils and carbuncles. If it spreads through the bloodstream, it can cause heart and lung infections, hepatitis, meningitis and even blood poisoning. Patients with a damaged skin barrier (neurodermatitis sufferers) and people with circulatory disorders of the skin are particularly at risk.
The Staphylococcus aureus strains, which are now resistant due to the excessive use of antibiotics (MRSA strains), are particularly problematic. The toxic shock syndrome (circulatory failure due to the explosion of staphylococci in the body) is also very dangerous for the patient. In addition, staphylococci can cause food poisoning, as even heat treatment does not completely kill the pathogen. Some strains are even insensitive to heat. Staphylococcus epidermidis likes to accumulate on foreign materials and, despite adequate disinfection, gets into the patient's body, where it can cause infections and even blood poisoning. Elderly people with heart disease and a weakened immune system and recently operated patients are particularly at risk. After amputations, the invading spheroidal bacteria delay the healing process.
Streptococci cause tooth decay by attacking tooth enamel and are responsible for many ENT infections such as otitis media and tonsillitis. They are also considered to be the cause of pneumonia, purulent inflammation of the connective tissue (phlegmon), pus lichen (impetigo), wound and urinary tract infections, scarlet fever, puerperal fever and Toxic Shock Syndrome (TSS).
Streptococci can usually be treated well with penicillin. Enterococci can lead to chronic urinary tract inflammation when they enter the urinary tract organs from the intestine. They can also cause inflammation of the pleura and the lining of the heart. They are treated with a combination of aminopenicillin and aminoglycosides or - in the case of resistance to penicillin or oxacillin - with a combination of ampicillin and gentamycin.