As Lewy body dementia is a form of dementia that can occur as an independent or secondary disease. As part of this neurodegenerative disease, Lewy bodies appear in the brain, which reduces the production of dopamine.
What is Lewy body dementia?

© Photographee.eu - stock.adobe.com
Lewy body dementia is named after the neurologist Friedrich H. Lewy, who first described the disease in a chapter of his book. The so-called Lewy bodies were discovered for the first time as part of Parkinson's disease. These are inclusions found in certain nerve cells other than the brain stem.
It has been known since 1989 that Lewy bodies can occur in patients who do not show any symptoms of Parkinson's disease. Lewy body dementia is the second most common dementia after Alzheimer's and cannot be cured. The disease usually begins at an advanced age; Lewy body dementia usually occurs between the ages of 50 and 83.
causes
With advancing age, protein clumps in the brain of some people, which over time lead to symptoms of failure. The Lewy bodies are made up of the protein alpha-synuclein, but it has not yet been clarified exactly what their role is in the human body. In Lewy body dementia, clumps of this protein form in the brain cells, with inclusions mainly occurring at the nerve endings. Since the signal is passed on there, failure phenomena occur for this reason.
Symptoms, ailments & signs
Those affected suffer from a progressive memory disorder, with alertness and mental ability fluctuating very quickly over the course of a day. Furthermore, the patients suffer from optical hallucinations and see animals or people, for example. Acoustic hallucinations, such as hearing noises or voices, are less common.
These psychotic symptoms are very difficult to treat with antipsychotics, as these are extremely poorly tolerated by many patients. The so-called Pisa syndrome or a very pronounced Parkinson's syndrome then often occurs. However, some patients have Parkinson's symptoms even without antipsychotic treatment. These include shaking hands at rest, muscle stiffness, walking in small steps and leaning forward, as well as reducing the movements of the facial expression.
In addition, there are behavioral disorders in REM sleep (dream sleep). Those affected then live out their dreams very strongly because they lack motor inhibition. They scream and talk in their sleep, lash out and fall out of bed. Many patients also suffer from depression, hypotonic circulatory disorders, and urinary incontinence. Most of the time, they fall frequently, and those affected can also lose consciousness.
The ability to find one's way in everyday life is also increasingly lost. The patients have great difficulty planning or carrying out actions and making decisions. The pace of work slows down and there is a reduction in the ability to concentrate and control of attention.
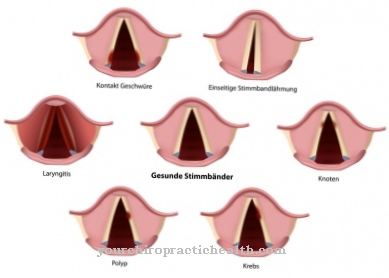
In the later course there are also impairments of speech, the patients become bedridden and in the end stage also swallowing disorders occur. Most of the time, those affected then die of pneumonia. Mixed forms are also possible, i.e. symptoms of Alzheimer's disease also occur. The symptoms that arise in the course of the disease process vary from person to person and depend on which areas of the brain are affected.
Diagnosis & course of disease
The doctor mainly bases the diagnosis on the typical symptoms that occur as part of this disease. It is important to think about this very special form of dementia, as many cases are often incorrectly diagnosed as Alzheimer's disease. Without the knowledge that psychotic symptoms have existed for a longer period of time, it can also be mistaken for delirium. Technical examination methods are not particularly helpful in the diagnosis of Lewy body dementia.
The electroencephalogram only shows unspecific changes, and magnetic resonance tomography (MRI) or computed tomography (CT) do not show any characteristic findings. With the help of a dopamine transporter examination, Lewy body dementia can be better differentiated from other forms. In the meantime, the focus is also on alternative therapies, such as cognitive or mental training.
If you strengthen your body and mind, you can significantly reduce the risk of developing dementia. After the diagnosis, the average duration of the illness is between six and eight years, but there are also very fast or very slow courses.
Complications
In Lewy body dementia, those affected suffer from the usual symptoms of dementia. These can significantly limit and reduce the quality of life of the person affected. It is not uncommon for patients to then rely on the help of other people in their everyday life and often pose a danger to themselves.
Above all, this leads to memory disorders and hallucinations. Those affected cannot distinguish which events occur in reality. Likewise, patients can hear voices from other people who are not there. It is not uncommon for Lewy body dementia to lead to circulatory disorders and incontinence. Patients also continue to suffer from depression and various behavioral disorders.
The sleep of those affected is not infrequently disturbed and there is a significant reduction in the patient's ability to concentrate. Lewy body dementia can also impair communication and lead to pneumonia. The treatment of Lewy body dementia can be done with the help of medication. However, not all complaints can be restricted, so that the course of the disease is not completely positive.
When should you go to the doctor?
Memory disorders should be examined more closely by a doctor even in the event of minor abnormalities. If there are problems with memory retrieval, memory impairment, or memory lapses, there is cause for concern. If no new knowledge can be acquired or if the person concerned is objectively reproducing false memories, a doctor is required. A loss of the usual level of performance and problems coping with everyday obligations should be examined and treated. If your hands are trembling, you have internal restlessness or problems with your muscles, you should consult a doctor.
Unsteady gait, dizziness or an increased risk of accidents should be discussed with a doctor. A leaning forward gait is a special feature of Lewy body dementia. As soon as relatives notice this in the affected person, they should work towards a doctor's visit. Reduced movement, restricted mobility or social withdrawal are further warnings that should be followed up. If incontinence, behavioral problems or circulatory problems occur, a doctor is required.
In the event of depression, mood swings or changes in personality, a doctor's visit is advisable. If the above-mentioned abnormalities gradually increase over a period of several months, a doctor should be consulted immediately. Concentration disorders, a decrease in the normal pace of work and problems with maintaining alertness must also be checked by a doctor.
Treatment & Therapy

Clozapine requires special precautionary measures such as constant blood counts. Parkinson's motor symptoms are very difficult to treat because patients with Lewy body dementia respond extremely poorly to Parkinson's medication and the psychotic symptoms are exacerbated. Small doses of L-Dopa are relatively well tolerated. The treatment of depression is done with so-called selective serotonin reuptake inhibitors (SSRI).
You can find your medication here
➔ Medicines against memory disorders and forgetfulnessOutlook & forecast
However, not all symptoms become apparent as the disease progresses. As it progresses, Lewy body dementia is characterized primarily by enormous fluctuations in the patient's mental performance and attention. There are more and more visual hallucinations that become more and more detailed. At the beginning of Lewy body dementia, patients can still distinguish between reality and hallucinations. However, they do not succeed in doing this at an advanced stage.
In addition, slight symptoms of Parkinson's disease become visible later, which are mainly reflected in the trembling of the hands, in the stiff movements and in the unsteady gait. Lewy body dementia often leads to pronounced insomnia and hyposomnia. This significantly disrupts the sleep-wake cycle. In the further course of the patient's illness, urinary and fecal incontinence usually occurs.
The risk of falling for the patient increases significantly due to the increasing limitation of movements. Falls lead to increased disturbances and loss of consciousness. In addition, increased fractures and other serious injuries occur, which in turn lead to further limitations for the patient. In the later course of the disease, the patient's weakness often increases as a result of such accompanying diseases. This leads to the further deterioration of the immune system.
prevention
So far it is not possible to protect yourself from Lewy body dementia. However, there are some factors that reduce the risk of developing this form of dementia. This includes physical, mental and social activity as well as a balanced diet rich in vitamins E, C and beta-carotene. The focus is on low-cholesterol and low-fat food intake. The preventive measures also include the treatment of cardiac arrhythmias, high blood pressure and diabetes mellitus.
Aftercare
For people with dementia, follow-up care consists of returning them to their home environment after an inpatient stay. The challenge is particularly evident in the need to rely on caring relatives, who first have to find their way into their new role. The follow-up care therefore not only affects the patient, but much more also their relatives, who need to be informed and looked after in order to avoid being overwhelmed.
A day-patient stay in a clinic can be useful to make things easier, because here the sick are gradually released into everyday life. A certain degree of autonomy can be regained through therapeutic offers, depending on the stage of dementia. It is important that those affected are not overwhelmed by the therapist, as this can lead to a renewed outbreak of the disease. The needs of each individual must be carefully considered.
If the patient then goes completely into the home environment, it is also helpful here to receive regular visits to the doctor or hire a professional nurse to provide support in the difficult initial period. Good everyday planning plays a major role so that the patient is challenged and there is no emptiness in which the disease can break out. Participation in social life, picking up on old hobbies and regular training of body and mind are just a few recommendations.
You can do that yourself
The creation of a weekly plan provides structure and thus security. The work to be done and important dates can be entered here. Signs on cupboards that point out the respective contents help with orientation in the apartment. Objects such as the key and the wallet are easier to find by assigning fixed locations. A piece of paper with important numbers right next to the phone ensures more safety in emergencies. A home emergency call system can also help. Clearly structured shopping lists with the name and the required quantity of the product are suitable for shopping. If cooking is made more difficult due to deficits in action planning, the use of recipes makes things easier.
Since dementia affects, among other things, the ability to react, driving a car should be avoided. Instead, car pools can be formed, public transport can be used or relatives can be involved. If the person concerned was active in sports, it is advisable to obtain information about group offers.
Maintaining familiar interests and processes for as long as possible has a positive effect on both body and mind. In the case of advanced courses, it is advisable to draw up a power of attorney. In the event that the person concerned is no longer able to do so, a person of trust is authorized to make decisions in medical matters, to regulate financial matters or to sign contracts.





















.jpg)


