The monoclonal gammopathy is a haematological disease. It is characterized by the fact that monoclonal antibodies are excessive. Monoclonal gammopathy affects the functioning of the immune system and can lead to anemia, hypercalcemia, blood sedimentation, hypergammaglobulinaemia or hypogammaglobulinemia and renal insufficiency, among other things.
What is Monoclonal Gammopathy?

© designua - stock.adobe.com
In the monoclonal gammopathy it is a hematological disease that affects the immune system. The defining feature of the clinical picture is the increased concentration of monoclonal antibodies, which occur in the so-called gamma fraction of proteins in blood serum.
Antibodies are substances in the human body that help the immune system to recognize and then fight against pathogens and foreign bodies. The addition "monoclonal" refers to the origin of these specific antibodies: The human body produces this type of antibody with the help of a cell clone. All cell clones of an individual are derived from one and the same cell, a so-called B lymphocyte.
causes
Monoclonal gammopathy can be traced back to various causes, which have in common that the crucial cell clone is changed. The affected cell clone multiplies in an uncontrolled manner and in this way causes various physical disorders.
A disease that can lead to monoclonal gammopathy is AL amyloidosis, which in turn may be due to other diseases such as Waldenström's disease, MGUS or a plasmacytoma. AL amyloidosis manifests itself in deposits of proteins inside and outside of cells. The result is a wide range of functional organ disorders and anatomical changes, for example in the form of edema, induration and other pathological phenomena.
Schnitzler syndrome can also lead to monoclonal gammopathy. Schnitzler syndrome is a rare disease in which monoclonal gammopathy is associated with chronic nettle rash (urticaria) and joint pain. B-cell lymphoma, non-Hodgkin lymphoma, pyoderma gangrenosum and other underlying diseases can also lead to monoclonal gammopathy.
Symptoms, ailments & signs
Certain symptoms are typical of monoclonal gammopathy; conversely, the presence of one, several or even all of the signs does not necessarily have to be due to monoclonal gammopathy: in any case, an individual and extensive diagnosis is required.
In many cases, monoclonal gammopathy leads to anemia, often referred to as anemia. This is a deficiency of the red blood pigment hemoglobin, which plays a central role in the transport of oxygen. As a result of anemia, symptoms such as dizziness, weakness, difficulty concentrating and many others can manifest themselves.
In the context of monoclonal gammopathy, hypercalcemia can also occur, which is characterized by a pathologically increased calcium level in the blood. Possible symptoms of severe hypercalcemia are loss of appetite, vomiting, nausea, constipation, mental symptoms, hypotonia, and others.
Abnormalities in the sedimentation rate or reaction (blood sedimentation) are also typical. In addition, monoclonal gammopathy can lead to hypergammaglobulinaemia or hypogammaglobulinaemia, i.e. to a significant increase or decrease in certain plasma proteins, namely gamma globulins.
Gamma globulins are also part of the immune system and play a role in the body's own recognition and defense against potentially harmful intruders. Furthermore, monoclonal gammopathy can lead to renal insufficiency.
Diagnosis & course of disease
When making a diagnosis, doctors first start with the symptoms and check whether there are typical symptoms of monoclonal gammopathy. If there is a suspicion, specific tests are possible. One of them is immunoelectrophoresis, which can detect the relevant antibodies in the blood serum.
Before that, serum protein electrophoresis determines the serum proteins present on a more general level. The course of monoclonal gammopathy can be very different, as the underlying disease plays an essential role in the chances of successful treatment and also has an impact on the overall severity of the clinical picture.
Complications
This disease is primarily characterized by severe anemia. As a result, those affected suffer from reduced resilience and severe fatigue. Certain everyday activities or sporting activities are no longer possible for the person concerned, so that there are significant restrictions in everyday life. It is not uncommon for sleep problems and disorders of concentration to occur.
A feeling of weakness also occurs and can reduce the patient's quality of life. Not infrequently, the patients also suffer from nausea, vomiting and thus also from a loss of appetite. The muscles are broken down and kidney failure can occur. This is usually fatal without treatment. The affected person is therefore dependent on a donor kidney or on dialysis in order to survive.
Treatment of the disease takes place with the help of radiation therapy or chemotherapy. Chemotherapy usually leads to various unpleasant side effects. The disease is not completely curable in every case, so that in some cases there is also a reduced life expectancy for the person affected. Damage to internal organs in particular is often irreversible and can no longer be treated directly.
When should you go to the doctor?
If health impairments such as dizziness, internal weakness, malaise or a decrease in mental or physical performance occur, a doctor should be consulted. If the daily requirements can no longer be met as usual or if concentration and attention are impaired, a doctor should be consulted. If you have flu-like symptoms such as vomiting, nausea, fatigue, exhaustion or an increased need for sleep, a doctor should be consulted. If the symptoms persist for several days or if they increase in scope and intensity, a medical evaluation is recommended.
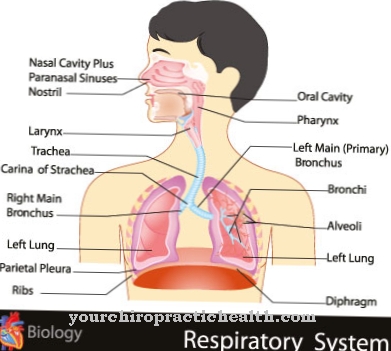
A doctor should be presented to a doctor if the amount of oxygen in the organism is reduced or respiratory activity is impaired. There is a risk of functional failure of the organs, which can lead to a life-threatening condition of the person concerned. A doctor should be consulted in the event of digestive tract disorders, constipation or a feeling of fullness. Changes to the toilet, decreased urine volume or discoloration of the urine should be examined and treated. A general feeling of illness or a decreased well-being are further signs of an irregularity. If, in addition to physical problems, the person concerned also experiences mental or emotional discomfort, a doctor's visit is also necessary. In the case of persistent or increasing mood swings, abnormal behavior or a depressed appearance, the person concerned needs medical help and medical care.
Treatment & Therapy
The treatment of monoclonal gammopathy depends on the cause, which is present in the individual case. The prospect of a successful therapy can vary widely and cannot be generalized. For AL amyloidosis due to a plasmacytoma or multiple myeloma, a bone marrow transplant may be an option, with which doctors try to treat the cause of the plasmacytoma.
More common options are chemotherapy and local radiation therapy, as well as various drug treatment approaches. Chemotherapy is also often an option for B-cell lymphoma. If the treatment of AL amyloidosis is successful, not only can the monoclonal gammopathy improve; The disorders and changes in the affected organs such as the kidneys, heart, liver or intestines may also be reversible.
However, this also depends on the individual case. If the monoclonal gammopathy is due to Schnitzler's syndrome, treatment with interleukin-1 antagonists may be an option. The nettle rash, which also occurs in this syndrome, is often hardly treatable; Options include PUVA therapy and non-steroidal anti-inflammatory drugs, with the latter also being used against joint and bone pain as well as fever attacks in the context of Schnitzler's syndrome.
You can find your medication here
➔ Medicines to strengthen the defense and immune systemOutlook & forecast
The prognosis of monoclonal gammopathy is based on the form and stage of the disease. The igM-MGUS offers a relatively poor prognosis, depending on any risk factors. All forms can develop into a serious illness over the course of years, which can be fatal for the patient. For example, malignant malignancies can appear in different places in the body. The likelihood of serious complications increases with age. Life expectancy is slightly lower than that of healthy people. There is a risk that the condition will develop into a chronic disease that significantly restricts the patient's daily life.
The prognosis is made by the responsible oncologist or another specialist with regard to factors such as the symptoms, the form of the disease and the age of the patient. Regardless of the prognosis, however, many sufferers can lead a relatively symptom-free life. The physical limitations usually develop slowly and do not significantly reduce the patient's quality of life. Only in the case of malignant diseases is a faster course with a progressive decrease in wellbeing to be expected. The malignant form of monoclonal gammopathy can be fatal.
prevention
Specific prevention of monoclonal gammopathy is not possible. Early detection and treatment of the causative disease can possibly prevent severe courses and create the basis for early therapy for monoclonal gammopathy.
Aftercare
Monoclonal gammopathies are usually protracted diseases that often require intensive follow-up care. The follow-up measures that need to be taken depend on the type and course of the individual illness. In many cases, the lymphomas are low-grade malignant and are classified as non-Hodgkin lymphomas.
Radiation and chemotherapy often do not lead to a complete cure for these lymphomas. However, the symptoms can be significantly alleviated, thereby improving the quality of life of those affected. Follow-up care includes regular examinations that record the patient's condition and at the same time determine further treatment.
In the event of a deterioration in health, it is also possible to react quickly. Even after successful treatment of the disease, further visits to the doctor should be made over a longer period of time, since recurrences can occur even after several years. However, lifelong follow-up is often necessary for monoclonal gammopathy.
This is especially true if the disease can no longer be cured using conventional treatment methods. In these cases, follow-up care is of a palliative nature. Due to the lengthy course of the disease, those affected often need psychological counseling, among other things, to prevent depression. For many patients, psychotherapy can therefore help to significantly improve their quality of life. Fears about the course of the disease and possible death are also often reduced.
You can do that yourself
The clinical picture of monoclonal gammopathy is complex and varied. For this reason, how the disease is dealt with in everyday life depends heavily on its cause, the therapy methods chosen and the symptoms present. Sufferers whose symptoms are caused by a malignant disease can turn to self-help groups and organizations for cancer. There their relatives can also find help in dealing with the sick person.
Since treating the underlying disease can put a heavy strain on the organism, it is advisable to strengthen the immune system. A balanced diet rich in vitamins plays an important role here. It is essential to avoid additional stress caused by heavy workload. In some cases there are no symptoms of the disease despite the presence of a monoclonal gammopathy finding. Those affected can also strengthen their immune system preventively. At least in the first year after the initial diagnosis, physical exertion and psychological stress should be avoided.
Regular medical checks are important. As soon as those affected notice physical symptoms, a doctor should be consulted and, if necessary, a new blood count should be taken. Otherwise, alternative healing methods can also be helpful in the case of monoclonal gammopathy and contribute to general physical relaxation. Even light exercise can help those affected.