Of the Neonator hemorrhagic disease is a blood clotting disorder that can affect infants and is due to a lack of vitamin K. Vitamin K is relevant for the synthesis of various coagulation factors. In order to treat the disease, the infant is given intravenous substitution of the necessary vitamin.
What is neonatorial hemorrhagic disease?

© AlionaUrsu - stock.adobe.com
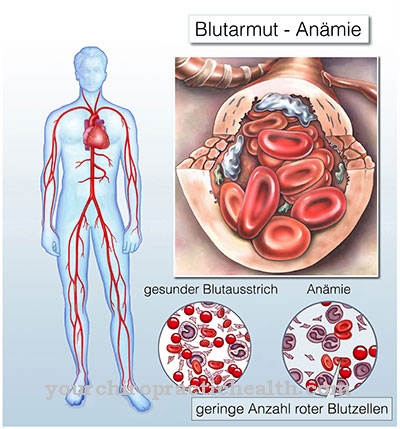
Blood clotting protects people from infection and extraordinary blood loss. The central element of coagulation is the so-called coagulation cascade, in which various endogenous and foreign substances are involved. Coagulation disorders can manifest themselves in a tendency to bleed. Often there is a genetic cause.
An external cause, however, is for the bleeding tendency of patients with Neonator hemorrhagic disease responsible. The age of onset of this pathological phenomenon is infancy. Thus, the complex of bleeding-related symptoms is called hemorrhagic disease in fetuses and newborns.
Those affected suffer from a so-called haemorrhagic diathesis, which manifests itself either as an abnormally long or abnormally heavy bleeding tendency in the event of an injury. Bleeding from inappropriate causes is sometimes referred to as a hemorrhagic diathesis. These three signs may be present at the same time.
causes
Vitamin K plays an important role in blood clotting. In the human body, the fat-soluble vitamin is involved in the production of various proteins. These proteins are primarily blood coagulation proteins, which are also known as blood coagulation factors. If there is not enough vitamin K in the body, the organism cannot adequately produce the coagulation factors required for clotting.
This connection determines the causal connection of the disease haemorrhagicus neonatorum. The primary cause of this coagulation disorder is a lack of vitamin K, which prevents the infant's body from producing enough coagulation factors for adequate blood clotting. The vitamin is especially relevant for coagulation factors II, VII, IX and X.
In addition to malnutrition in the mother during pregnancy, anticonvulsant therapy with drugs such as hydantoin and primidone can lead to such a deficiency in the newborn's organism. Antibiotic treatments during pregnancy can also be the cause. If the deficiency does not exist from birth, the infant is often preceded by parenteral nutrition.
Symptoms, ailments & signs
In most cases, neonatorial haemorrhagic disease is present from birth. The phenomenon rarely occurs due to influences after pregnancy. However, if the vitamin K deficiency is present from birth, it does not have to manifest itself immediately after birth. In most cases, the coagulation disorder manifests itself in a kind of early form at least within the first week of life.
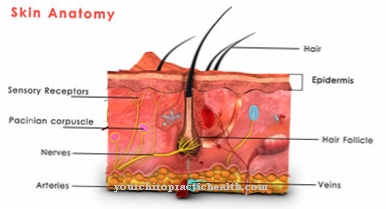
In this early form, neonatorum haemorrhagic disease becomes noticeable between the third and seventh day of life of the newborn in the form of a cephalhematoma. Other unexplained bruises on the skin can also be signs. For example, the dermal lesions indicate intracranial bleeding. In addition, bleeding of the skin and gastrointestinal bleeding may occur. There is no obvious reason for the bleeding.
If neonatorum haemorrhagic disease is not present from birth, it is usually due to a reduced concentration of vitamin K in breast milk. The late form of coagulation disorder acquired in this way becomes noticeable in the first three months of life as a tendency to intracranial bleeding.
Diagnosis & course of disease
The diagnosis of neonatorial haemorrhagic disease is often made by the doctor in the first week of the baby's life. The main reason for suspicion of a coagulation disorder are the bruises on the skin. Laboratory diagnostics show a prolonged prothrombin time in the form of an abnormal Quick value.
Both the bleeding time and the partial thromboplastin time are usually found to be normal in the laboratory. Haemorrhagicus neonatorum disease is to be distinguished from other coagulation disorders. This differential diagnostic delimitation is mainly achieved by determining the vitamin K values. The prognosis for the patients is excellent.
Complications
With neonatorum haemorrhagic disease, those affected suffer from bruises that can appear all over the body.The symptoms can often be felt a few weeks after the birth and are not associated with the effects of violence on the body. They usually occur spontaneously and inexplicably. Bleeding between the skin can also occur.
Those affected suffer from pain, which can be expressed by screaming, especially in children. As a rule, self-healing does not occur, so treatment of neonatorial haemorrhagic disease by a doctor is definitely necessary. In some cases, the child's parents also suffer from mental health problems, as they cannot identify the cause of the bruising in the first place.
In most cases, neonatorum haemorrhagic disease is treated with the addition of vitamins and blood transfusions. There are no further complications. In the worst case, however, it can lead to bleeding in the brain, which can be fatal. For this reason, it is important to identify the source of the bleeding and to stop the bleeding so that these complications do not occur. However, neonatorum haemorrhagic disease does not usually reduce life expectancy.
When should you go to the doctor?
Haemorrhagicus neonatorum disease normally only occurs in newborns. Since infants belong to the risk group due to their natural incapacity to act, parents should show increased vigilance. Newborns are always examined intensively by the obstetricians present immediately after birth.
Existing irregularities or anomalies are noticed and documented. Necessary medical care is taken over by the trained staff in routine processes. The same procedure can be guaranteed for a birth in a birthing center or for a home birth with a midwife present. Therefore, parents do not need to take action in these cases.
If a spontaneous delivery takes place without an obstetrician, the mother and child should be transported to the nearest hospital as quickly as possible. If the first symptoms appear a few days after delivery, a doctor is required. Bruising, bleeding or discoloration of the skin's appearance indicate an existing irregularity that must be examined and clarified.
Open wounds must be treated sterile so that no germs can get into the organism. In the worst case, there is an alternative risk of sepsis and thus a potential risk to life for the child. Circulatory disorders, pain or behavioral problems in the newborn should be presented to a doctor. A doctor should be consulted immediately if there are disorders of the heart rhythm, palpitations or refusal of food.
Treatment & Therapy
Unlike many other coagulation disorders, neonatorum haemorrhagic disease can be treated causally. The phenomenon is therefore considered to be curable and usually does not require much more than a substitution of the missing vitamin. In most cases, the substitution therapy measure consists of intravenous substitution.
If the deficiency is not extremely pronounced, a dose of one to two milligrams of the vitamin is sufficient for the causal treatment. The intravenous administration of the vitamin prevents insufficient absorption by the child's intestinal flora. A blood transfusion is only required in extremely rare extreme cases. The blood values relevant for coagulation are determined closely during therapy.
Usually, blood clotting stabilizes within days. If bleeding has occurred in the internal organs, medical intervention may also be required to stop the source of the bleeding. Bleeding in the brain would be a fatal complication, as it could result in symptoms similar to a stroke. Cerebral haemorrhage usually does not occur in the context of neonatorial haemorrhagic disease.
Outlook & forecast
The earlier the existence of the disease haemolyticus neonatorum was recognized, the better the prognosis and the better the chances of recovery. In many of the sick children, the disease goes away without treatment or with the use of light therapy alone. Nevertheless, in a few particularly serious cases, the disease can develop into life-threatening proportions. This is especially the case when there is no suitable therapy. Then there is the possibility that sick children may die from the dreaded complications of the disease.
Without therapy, the steadily progressing hemolysis leads to dangerous hyperbilirubinemia directly after birth and thus leads to damage to the child through indirect bilirubin. Muscle weakness especially occurring in newborns can indicate the onset of encephalopathy.
With the increasing damage to the brain, those affected develop generalized spasticity and seizures. Often there are also respiratory failure and pulmonary bleeding. About 25% of the affected fetuses develop signs of pronounced anemia with dangerous hemoglobin concentrations of less than 8 g / dl between the 18th and 35th week of pregnancy due to the anti-D.
If left untreated, this leads to hypoxia, acidosis, liver damage, and enlargement of the spleen. Which in turn leads to a massive tendency towards edema in the diseased fetus. In addition, other complications such as pulmonary edema and pulmonary bleeding can lead to an early death.
prevention
Haemorrhagicus neonatorum disease can be prevented. As a preventive measure, an infant is given vitamin K supplements as standard after birth. The vitamin is administered once between the third and tenth day of life and is repeated around the 28th day of life.
Usually the amount of the substituted vitamin corresponds to the recommended two milligrams. Since this preventive measure has long since become standard in hospitals, neonatorum haemorrhagic disease now only occurs in rare cases.
Aftercare
In most cases, the affected person does not have any special or direct follow-up measures available in the case of neonatorial haemorrhagic disease. For this reason, early diagnosis of this disease is important in order to avert the occurrence of complications and complaints in good time. If the person concerned wishes to have children, he or she should seek genetic testing and counseling in order to prevent recurrence in the children.
The disease can be treated relatively well with the help of various medications and supplements. The person concerned should always pay attention to the correct dosage and also to a regular intake in order to alleviate the symptoms correctly and permanently. Regular checks of the internal organs and blood values are also very important in order to detect other complaints at an early stage.
In the event of various treatments or surgical interventions, the person concerned should always inform the doctor about the disease neonatorum haemorrhagicus so that there are no complications. Further follow-up measures are usually not available to those affected with this disease. Neonatorum haemorrhagic disease may reduce the patient's life expectancy, although no general prediction can be made.
You can do that yourself
Since the bleeding time is significantly longer due to the lack of vitamin K, the sick child must be treated with special care. All nursing activities, such as carrying around, rocking or changing the child, should be reduced to a necessary minimum so as not to provoke new bleeding. Strong pressure on a body region or part of the body must be avoided as a matter of urgency in order not to injure the smallest vessels.
The skin should be monitored regularly for so-called petechiae (the smallest of skin bleeding) or large bruises. The stool should also be checked for irregularities, such as fresh blood deposits or digested blood (tarry stools). The black tarry stool in particular can, however, be confused with ordinary meconium, also known as child speck.
Once the corresponding blood parameters have normalized again, the newborn can be cared for and touched again as usual. It is crucial that the child receives the standard dose of vitamin K, which is administered after birth on the 3rd, 10th and 28th day of life. Corresponding medical appointments must urgently be kept. The pediatrician will also point this out again.


.jpg)