The myotonic dystrophy type 1 (Curschmann-Steinert syndrome) is an autosomal dominant inherited multisystem disease with the main symptoms of muscle weakness and opacity of the lens (cataract). A distinction is made between two forms of the disease: an inborn (congenital) form, in which the newborn is noticeable due to muscle weakness ("floppy infant"), and an adult form, which only manifests itself in the 2nd to 3rd decade of life. Myotonic dystrophy type 1 is incurable and, depending on its severity and progression, shortens life expectancy.
What is myotonic dystrophy type 1?
© peshkova - stock.adobe.com
The myotonic dystrophy type 1 is one of the so-called trinucleotide repeat diseases. In the genetic code on the long arm of chromosome 19, a trinucleotide from the nucleobases cytosine, thymine and guanine is duplicated.
While this basic triplet is repeated 5-35 times in healthy people, in those with mild symptoms it is about 50-200, in severe forms even over 1000 repetitions. The trinucleotide does not directly code for a protein, but it does affect the synthesis of other proteins. An enzyme required in skeletal and cardiac muscles, dystrophia myotonica protein kinase (DMPK), is produced in a reduced manner due to the genetic defect.
But other proteins are also affected, e.g. the SIX5 expressed in the lens or the insulin receptor. Therefore, myotonic dystrophy type 1 affects many different organ systems. With an incidence of about 1: 20,000, myotonic dystrophy type 1 is the most common myotonia and at the same time the most common muscular dystrophy that occurs in adulthood.
In terms of inheritance, the number of trinucleotide repeats increases from generation to generation, so that the onset of the disease in the offspring is earlier and more severe. The congenital form is always inherited from the mother. Myotonic dystrophy type 1 affects boys more frequently than girls.
causes
In the congenital form, the infant is noticeable immediately after birth with generalized muscle weakness, a raised upper lip and respiratory failure. Because of the breathing problems, many newborns are dependent on artificial respiration and 25% -50% die within the first 18 months of life.
Developmental delays and severe mental retardation are to be expected in children who survive longer. Their life expectancy is around 30-40 years. If the disease only breaks out in adulthood, those affected often first notice muscle weakness in muscles distant from the torso, especially in the legs, neck and face area. The facial muscles atrophy, making the patient look gaunt.
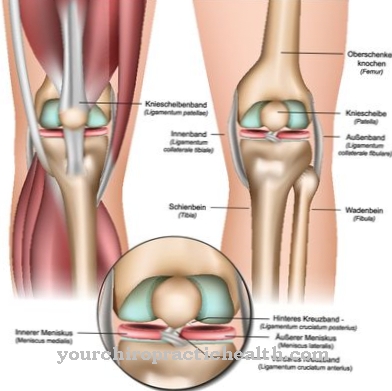
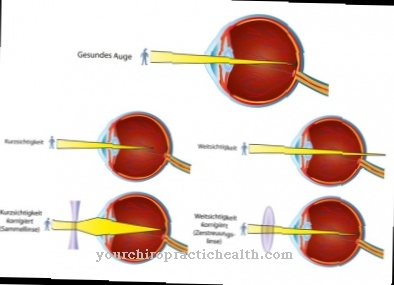
Speech and swallowing disorders also result. The muscle weakness is accompanied by delayed muscle relaxation, so that it is difficult for those affected, for example, to loosen a movement again. Further symptoms are lens opacity, inner ear hearing loss, an increased need for sleep, cognitive limitations and reduced glucose tolerance up to diabetes mellitus. Due to the disturbed hormonal balance, testicular atrophy and baldness typically occur in men, and menstrual disorders in women.
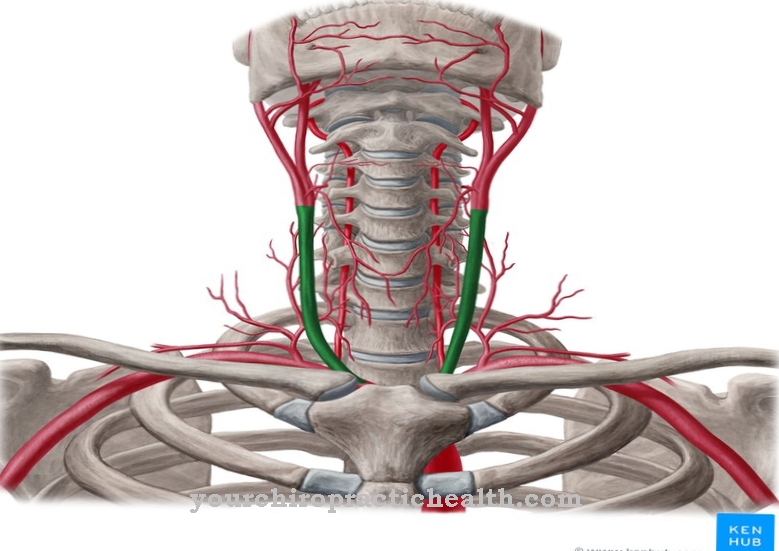
The effects on the heart muscles are particularly dangerous: cardiac arrhythmias often occur, and occasionally even cardiac arrest. If the muscle weakness reaches the core muscles, breathing disorders and an increased susceptibility to infections of the lungs are the result. Type 1 myotonic dystrophy is always progressive, but the severity and composition of its symptoms are extremely variable. On average, life expectancy in the adult form of myotonic dystrophy type 1 is around 50-60 years.
Symptoms, ailments & signs
The main characteristic of type 1 myotonic dystrophy is the delayed relaxation of the muscles after a muscle contraction. This characteristic can be used to distinguish the disease from other muscular dystrophies. The muscles furthest from the trunk, such as the face, neck, forearm, hand, lower leg and foot muscles, are particularly affected. There are other symptoms independent of the muscle complaints.
Cardiac arrhythmias or cardiac insufficiency often occur. Due to the involvement of the heart, anesthetic incidents often occur during anesthesia. Cataracts and balding hairs in men are often observed. The testosterone level is too low, which often leads to testicular loss. There is an increased risk of developing diabetes.
Speaking and swallowing are difficult for the patient. In addition, the patient is constantly tired during the day, which can lead to breathing pauses at night. However, sleep apnea is not always present. Digestive disorders, gallbladder disorders or hearing disorders can also occur as further symptoms. Although it is a hereditary condition, symptoms do not appear in many patients until they are 20 years old.
A cataract is often diagnosed as the first sign of the disease.However, there is also a form of the disease that exists from birth. This congenital form of muscle myotonia is characterized by a particularly severe course with life-threatening respiratory insufficiency and mental and physical developmental disorders.
Diagnosis & course
If you suspect myotonic dystrophy type 1 molecular genetic methods are used to diagnose the disease beyond doubt. These help rule out differential diagnoses with similar symptoms, e.g. myotonic dystrophy type 2. The diagnosis can be supported by electromyographic examinations (EMG). In those affected, typical patterns of spontaneous activity can be found, especially on the muscles distant from the torso. It is also important to have a thorough family history, also in order to provide further advice to the family.
Complications
With this disease, those affected mainly suffer from severe muscle weakness and symptoms that occur in the eyes. This leads to cataracts and clouding of the lens, so that the affected person's eyesight deteriorates significantly. In the worst case, it can also lead to complete blindness.
The quality of life is significantly reduced. Young people in particular can develop psychological complaints or depression if they have sudden visual problems or if they are blind. Furthermore, heart problems can occur, so that the patient can die of sudden cardiac death. It is not uncommon for those affected to suffer from diabetes.
The muscle weakness significantly limits the everyday life of those affected, so that in some cases they are also dependent on the help of other people. Certain activities or sports can no longer be carried out without further ado. The development of children is significantly restricted by the disease, so that complications can arise in adulthood. It is not possible to treat this disease causally.
However, many complaints can be restricted and alleviated so that everyday life becomes bearable for the person concerned. As a rule, there are no particular complications and the patient's life expectancy is not restricted by the disease.
When should you go to the doctor?
A doctor's visit is necessary as soon as the person concerned experiences impairments in coping with everyday life. A weakness in muscle strength, a decrease in physical performance and a loss of tissue are signs of a health disorder. If normal sporting activities can only be practiced to a limited extent or not at all, the observations should be discussed with a doctor. Various examinations must be initiated so that the cause can be clarified and a treatment plan drawn up.
A delay in voluntarily controlled muscle tension and decreased vision are worrying. If your vision is blurred or the lens is cloudy, a doctor's visit is advisable. An irregularity in the natural grip function is a warning signal from the body that requires action. An increased risk of accidents and falls must be discussed with a doctor so that countermeasures can be initiated. Disorders of the heart rhythm, palpitations or sleep interruptions should be examined more closely by a doctor.
If concentration or attention deficits occur or if reduced mental performance is noticed due to the impairment, a doctor's visit is necessary. If men suffer from decreased sexual desire or if they develop a bald head, a doctor should be consulted. If there are also emotional or mental stressful states, the affected person is threatened with consequences. They are to be prevented in good time.
Treatment & Therapy
A causal treatment of the myotonic dystrophy type 1 can not. Therapy focuses on symptom relief, e.g. through surgical treatment of the cataract, drug adjustment for cardiac arrhythmias or technical respiratory support. Physical therapy support can delay the progression of myotonic dystrophy type 1.
You can find your medication here
➔ Medicines for muscle weaknessOutlook & forecast
The prospects of diagnosed type 1 myotonic dystrophy are poor. Both life expectancy and quality of life suffer. Most patients don't even reach the age of 60. Many of them die from heart failure or succumb to infections. Therapeutic measures can often only marginally alleviate the symptoms of the disease. The genetic defect itself is not curable according to the current state of science. Many of those affected show signs of myotonic dystrophy type 1 before they are 20 years old. Others only see a doctor at an advanced age. Within families, there is an increased risk of the disease being inherited.
The suffering increases continuously as myotonic dystrophy type 1 progresses relentlessly over the years. Because of the weak muscles, those affected find it increasingly difficult to cope with everyday life alone. You need help. The musculoskeletal system comes to a standstill. After a while, a learned profession can no longer be pursued. The therapeutic approaches of drugs and physiotherapy increasingly lose their effectiveness over time. It is not uncommon for the physical decline of myotonic dystrophy type 1 to be accompanied by psychological problems.
prevention
Since the myotonic dystrophy type 1 If it is an inherited genetic defect, prevention is not possible.
Aftercare
Myotonic dystrophy type 1 is hereditary. According to the current state of research, a cure is not possible. The disease reduces life expectancy by around 50 years. Follow-up care is advisable to help slow the progression of dystrophy. Further goals of aftercare are to relieve symptoms and maintain quality of life.
During the follow-up, the tolerance of medication is checked if it has been administered to the patient. Follow-up care primarily relates to physical complaints. The mobility of the limbs should be maintained as long as possible through appropriate exercises. Accompanying psychotherapy can also be appropriate or even necessary.
An inadequate quality of life due to dystrophy can affect the patient's soul. The risk of depression is very high. With psychotherapy there is an opportunity to talk about negative feelings. At an advanced stage, a wheelchair may be required. During the aftercare, the sick person learns how to use the device on a daily basis.
Myotonic dystrophy also affects the heart function. A pacemaker counteracts the process. Follow-up treatment is carried out by a cardiologist. He monitors the healing process after the operation. The control will be discontinued when healing has proceeded as expected.

.jpg)


.jpg)








.jpg)




.jpg)


