At a Mycetoma or the Maduras mycosis it is a soft tissue infection caused by fungi or fungal bacteria. The infection occurs mainly in the arid areas of the tropics. The infection occurs via small injuries to the skin, through which the pathogens penetrate the organism.
What is a mycetoma?
.jpg)
© oatautta - stock.adobe.com
The was first described Maduras mycosis in the Indian province of Madura, hence the name of the infection. Since the infection usually occurs on the foot - the pathogen typically penetrates the organism through small cracks that occur when walking barefoot - the infection is also known as "Madurafuss".
Madura mycosis occurs in two different forms. The real mycetoma (Eumyzetoma) is caused by yeast or molds, the actinomycetoma (actinomycetoma) by different types of bacteria (Streptomyces, Actinomadura, Nocardia).
Overall, madura mycosis occurs very frequently around the world, with a geographical focus. While in Asia and Africa maduramycosis usually occurs in the form of eumycetoma, actinomycetoma is widespread in Mexico.
causes
The cause of madura mycosis is an infection with a fungus or a bacterium.
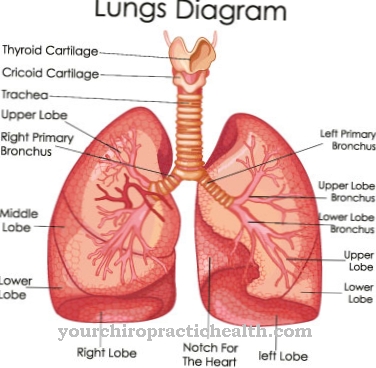
An infection usually occurs through wood prickly pounds that have entered the foot or through the penetration of fungi or bacteria through small injuries to the foot. The following fungi are possible pathogens for a eumycetoma: All fungi of the genus Madurella, the genus Acremonium, Phialophora verrucosa and Aspergillus flavus.
Different bacteria can be identified as the source of an actinomycetoma, namely different species of the bacterial genus Nocardia (especially Nocardia brasiliensis), different species of the genus Streptomyces (especially Streptomyces madurae) and Actinomadura.
Fungi are responsible for an infection in around 40% of all cases, 60% of all infections are due to an infection with bacteria.
Symptoms, ailments & signs
After an incubation period of a few weeks to several months, so-called granulomas develop on the infected soft tissue areas. These are painless nodules that contain the respective pathogen in the form of granular material. At the location of the nodules, there is also massive swelling of the affected part of the body. The purulent granules are transported to the outside via fistulas.
Various fungi or bacteria that enter the body through small skin injuries are possible pathogens. The feet are often infected because walking barefoot in various groups of the population causes the pathogens to get into a wound on the foot via wood splinters. The mycetoma is seen less often on the back, knees or hands.
Despite different pathogens, the symptoms of the disease are similar, so that the term mycetoma can be understood as a collective term. However, depending on the two groups of pathogens, there are not only similarities but also differences in symptoms. In a real mycetoma (fungal infection), for example, the nodules are not clearly delimited from one another. There are also many fistulas.
Furthermore, the bones are often involved very early in this form of infection. It is therefore often necessary to surgically remove the affected tissue areas in addition to the drug treatment. In the infection caused by bacteria (actinomycetoma), the granules are encapsulated from one another, with only a few fistulas forming. Bone involvement is less common here. Therefore, in an actinomycetoma, surgical removal of the affected tissue is rarely necessary.
Diagnosis & course
An initial diagnosis at Maduras mycosis can mostly be taken due to the clear symptoms. Painless small nodules and massive swelling of the infected area form. From the nodules or swellings, granular secretions are emptied - often without external influence.
The doctor clearly recognizes an infection after a microscopic examination. The secretion that has escaped is examined. If it is a fungal infection, the secretion has a granular, thread-like, white to slightly yellowish structure.
After a clear diagnosis, the doctor has a selection of different drugs that can be used for therapy. If drug therapy is applied in good time, the course of the infection is quite harmless and, above all, painless.
If madura mycosis, especially the eumycetoma caused by fungi, is not treated, the infection is chronic. Symptoms such as purulent growths do not heal on their own. In addition, an attack on other parts of the body is almost inevitable. In the worst case, the affected body regions have to be amputated.
Complications
An infection with the fungi of the mycetoma can lead to an additional bacterial superinfection. This means that another disease caused by bacteria is favored. This can also occur after medical treatment has been given.
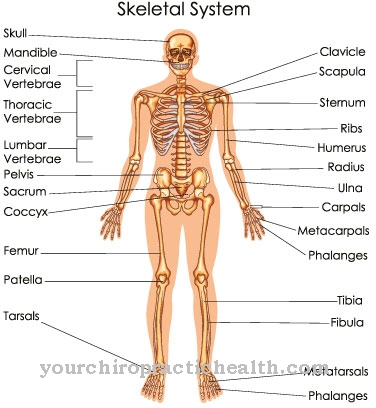
In most cases, however, complications with a mycetoma arise from a lack of medical treatment, as the tumor then has the opportunity to infiltrate the inside of the body and continue to grow inside. This can lead to bone destruction, which means that bone tissue is destroyed. The muscle tissue can also be affected. Adenopathy is also possible.
This is a disease of hormone-producing glands. Tumors caused by proliferating granulation tissue can form cerebral and visceral metastases. This refers to offshoots in the brain and internal organs.
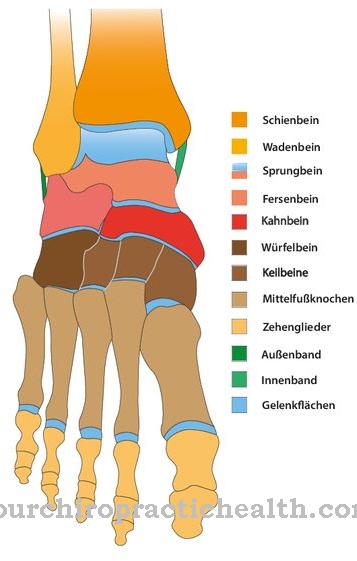
If the mycetomas are allowed to grow too long, since they occur frequently on the feet in particular, they can severely limit the ability to walk. Deformities of the ankles can lead to additional movement disorders. If joints, bones and muscles have been damaged too much, an amputation must be carried out, which leads to further disabilities.
When should you go to the doctor?
Changes in the appearance of the skin, discoloration or lump formation should be presented to a doctor. If the symptoms spread or if the intensity increases, there is a health impairment that must be examined and treated. If there is swelling, itching or open wounds, the cause should be clarified. A doctor should be consulted if the disturbances restrict the possibilities of movement or if there is a decrease in mobility. If the symptoms increase rapidly within a few hours, a doctor's visit is required as soon as possible.
The pathogens spread quickly and the body's own defense system is not strong enough to defend itself against it to the extent necessary. A decrease in physical performance, internal weakness or a general malaise indicate irregularities that should be presented to a doctor.If the person concerned suffers from the visual changes in the skin or the blemish, surgical removal of the unwanted tissue is necessary.
If there is inflammation of the skin, enlargement of an existing wound or gangrene, consult a doctor immediately. In severe cases there is a risk of sepsis and thus a potential threat to life. Irritability, behavioral problems or withdrawal from usual social activities are further indications of an existing illness.
Treatment & Therapy
A treatment of a Mycetoma takes place by means of drug information. In order to choose the right remedy in the right dosage, an accurate diagnosis is necessary. If there is a fungal infection, various antimycotics are used to treat it.
Since many of the fungal cultures are now very resistant or resistant to the antifungal agents, it is essential to control the effect while taking the medication. The funds are usually taken over a very long period of time, usually a few years.
In addition to administering medication, it is advisable to surgically remove the affected swollen or purulent areas in order to alleviate the associated discomfort for the patient.
If the mycetoma is triggered by bacteria, the patient is given an antibiotic. Even with a bacterial infection, it can happen that the swellings in the affected areas of the body do not heal. Even then, surgery would be indicated.
Outlook & forecast
Nowadays a mycetoma is easily treatable and offers a positive prognosis. The condition must be treated surgically or with medication to prevent the fungus from spreading. If left untreated, madura mycosis can develop into a chronic disease that is associated with numerous restrictions in professional and private life for the patient.
Amputations may be necessary during the course of the disease, which significantly reduce the patient's quality of life. As a result of an amputation, mental illnesses can also develop. For example, after losing a part of their body, some patients develop depression or anxiety disorders that require treatment. Physical complaints such as circulatory disorders or phantom pain also occur after an amputation and influence the assessment of the course.
The prognosis is good, however, as a whole range of therapy methods are available nowadays and the fungal disease is usually not fatal. The course of the disease is assessed by the responsible dermatologist or internist, who takes into account the severity of the disease, the patient's constitution and social factors such as the financial situation of the person concerned. If necessary, the prognosis must be adjusted, especially in the event of unforeseen complications, such as those that occur in particular with serious illnesses.
prevention
One Mycetoma can be prevented very easily. In the areas where the mycetoma is widespread, you should consistently avoid going barefoot. Should small injuries occur in the area of the foot, the wounds must be disinfected immediately and permanently. When traveling to corresponding areas, disinfectants or alcohol swabs should therefore not be missing in the first-aid kit.
Aftercare
Follow-up care for a mycetoma depends on the type of treatment and the success of the treatment. If the fungal attack can be treated with medication, medical follow-up is usually no longer necessary. If the infestation is not serious and treatment is timely, consequential damage can almost always be prevented.
In more severe cases, however, surgical interventions can be considered. It is aimed at removing infected tissue. In some cases, little tissue is removed, and good wound care is then important. Depending on the case and indication, preventive antibiotic therapy can be useful.
Follow-up examinations of the tissue for any remaining pathogens are also important. The follow-up care must be communicated by the specialist and depends on the severity of the procedure. Wound healing can be achieved within a few weeks with good wound care. Further aftercare measures are not necessary after the complete healing.
On the other hand, if the patient is amputated because too much tissue is involved, follow-up care is more difficult. The stump needs to be treated. If necessary, further therapies are added to the follow-up care. This is the case, for example, when the person concerned experiences phantom pain. Learning how to move in spite of the amputated body part is also part of the aftercare. The mentioned aftercare measures apply to eumycetomas caused by fungi as well as to actinomycetomas caused by bacteria.
You can do that yourself
A mycetoma is usually treated with medication. What measures the person affected can take to alleviate the symptoms and promote the healing process depends on the type and severity of the disease.
In principle, rest and bed rest apply. Especially in the first days of the illness, care should be taken to ensure that the bed is warm enough to avoid spreading the pathogen. In addition, swollen or purulent areas should be carefully cared for and treated with gentle care products if necessary. The use of such preparations should first be discussed with the responsible doctor. Surgical intervention is necessary if the symptoms are severe. After an operation, the skin is usually very irritated and must not be exposed to harmful influences such as dirt or allergens. The person affected should strictly adhere to the medical guidelines and inform the doctor about any unusual symptoms.
Mycetoma usually heals well provided it is treated early and a doctor monitors its progress. In order to avoid re-infection, the causes of the first fungal infection must be determined. For this purpose, a complaint diary can be created in which possible triggers and other abnormalities are noted.

.jpg)




















.jpg)

.jpg)
