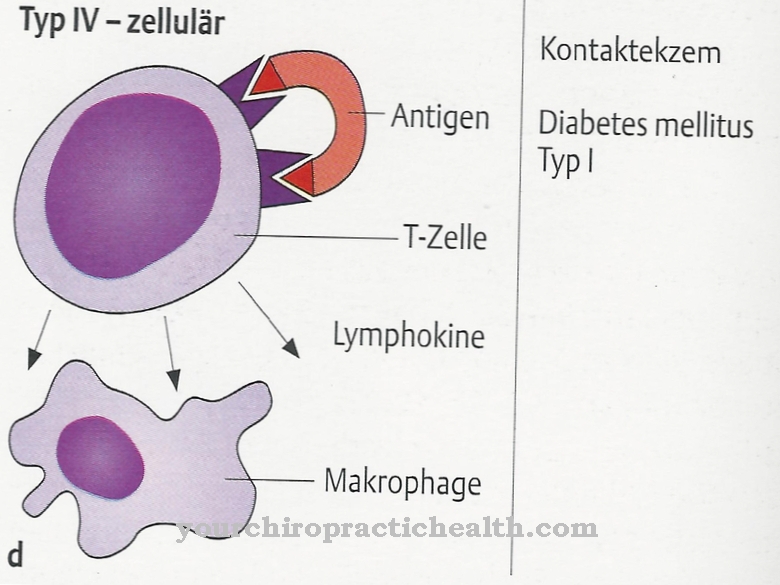
In the Neuromyelitis optica It is an autoimmune inflammatory disease that affects the central nervous system and leads to the degradation of certain insulating nerve sheaths (medical name demyelination). As a result, an inflammation of the optic nerve develops between a few months and two years. This occurs either on one side or on both sides. In addition, the spinal cord becomes inflamed (myelitis).
What is Neuromyelitis Optica?

© Martha Kosthorst - stock.adobe.com
In the Neuromyelitis optica In numerous cases there are special antibodies against a specific water channel, the so-called aquaporin-4 channel. The pathophysiological significance of these substances has not yet been fully clarified and is the subject of current medical research. The disorder is considered synonymous in some cases Devic Syndrome or with the abbreviation NMO designated.
It is a relatively rare disease of the central nervous system. Neuromyelitis optica accounts for around one percent of all demyelinating diseases. In addition, the question is whether neuromyelitis optica is a special form of multiple sclerosis or whether it is an independent disease.
The disease was scientifically described for the first time at the beginning of the 19th century. Eugène Devic and Fernand Gault then researched the disease, so that neuromyelitis optica is sometimes also referred to as Devic's syndrome. There is currently a study group dedicated to research into neuromyelitis optica. The topic is the networking of scientific and clinical findings to investigate the clinical course of the disease and its frequency.
causes
According to the current state of knowledge of medical research, there is still no complete clarity about the causes that lead to the development of neuromyelitis optica. However, it is assumed that special antibodies against the so-called aquaporin-4 channels play a central role in the development of the disease. Because these antibodies show up in numerous patients who are affected by neuromyelitis optica.
Symptoms, ailments & signs
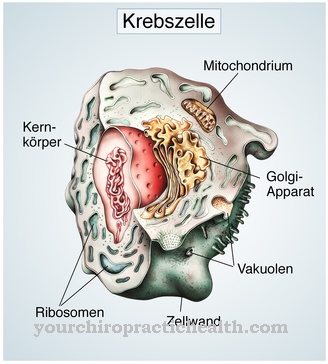
Neuromyelitis optica is associated with numerous typical symptoms and complaints. The first characteristic of the disease is that the myelin layer is broken down by central nerves. In connection with this, the neuritis nervi optici and the spinal cord are reduced.
In the further course of the disease, visual disturbances appear, which in some cases lead to blindness (medical name amaurosis). Blindness shows up in either one or both eyes and develops within a few hours or days. In addition, a paraplegic syndrome is possible in the context of neuromyelitis optica, which is associated, for example, with sensory disorders, paralyzed extremities or disorders of the bladder function.
Basically the disease shows either a monophasic or a multiphasic course. In addition, it may progress chronically. Histological examinations show some demyelinating foci that are similar to multiple sclerosis. Irreversible necroses are also possible.
Diagnosis & course of disease
If symptoms typical for neuromyelitis optica appear, a suitable specialist should be consulted immediately. He or she will discuss the patient's medical history (anamnesis) and the individual complaints with the patient concerned. This enables a clinical diagnosis to be made.
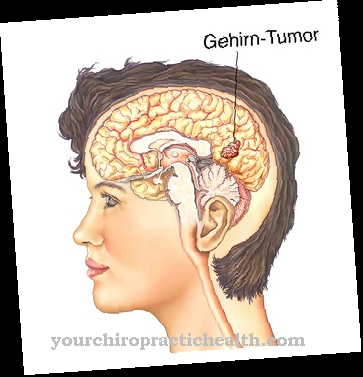
In connection with this, various neurological examinations are necessary in which, for example, inflammations in the optic nerves and the spinal cord are searched for. Damage to the brain, which in some cases shows similar symptoms, must also be excluded. The aquaporin-4 antibodies are determined to ensure the diagnosis.
Magnetic resonance imaging of the skull and the spine is also required. For example, multiple sclerosis and retrobulbar neuritis can be ruled out as part of the differential diagnosis. It should be noted that, especially at the beginning of the disease, an exact differentiation from multiple sclerosis is not always possible. Retrobulbar neuritis is often associated with visual disturbances similar to neuromyelitis optica, but without involvement of the spinal cord.
Complications
As a rule, neuromyelitis optica causes inflammation of the optic nerve. Therefore, if left untreated, the patient may experience complete loss of vision. Especially in children or young people, loss of vision can lead to severe psychological damage or even depression.
In children, neuromyelitis optica clearly disrupts development. As a rule, it cannot be universally predicted whether the loss of vision will occur on both sides or on one side. Furthermore, neuromyelitis optica can cause other disorders of sensitivity or paralysis in different parts of the body. The function of the bladder may be disturbed as a result, so that the patients develop incontinence.
Neuromyelitis optica can be treated with medication. If the affected person has lost sight, it cannot be restored and the vision loss is usually irreversible. If there are psychological complaints, the person concerned is dependent on psychological treatment. There are usually no complications. The life expectancy of the patient is also not negatively affected by neuromyelitis optica.
When should you go to the doctor?
Difficulty seeing or having pain in one or both eyes suggests an eye disease. A doctor must determine whether this is neuromyelitis optica and, if necessary, initiate further measures. The help of a doctor is necessary at the latest when well-being is impaired or further physical complaints occur in the muscles, intestines and bladder. People who already suffer from a chronic disease of the nerves should contact the responsible doctor quickly if the symptoms mentioned occur.
People with gastrointestinal diseases or neurological disorders are also best to speak to a specialist as soon as possible so that the optic neural myelitis can be recognized and treated before further complications occur. Apart from the family doctor, you can also speak to an ophthalmologist. Accompanying bladder and bowel incontinence must be treated by a gastroenterologist or another internist. If a muscle disease occurs, an orthopedic surgeon or a sports doctor should also be called in. In the long term, the sick often also need therapeutic support.
Treatment & Therapy
There are various options for treating neuromyelitis optica. These are used depending on the individual case and are based on the individual symptoms and the severity of the complaints. In numerous cases, the neuromyelitis optica runs in one episode, so it is monophasic.
On the other hand, a multiphasic or chronic course of the disease is also possible. The foci of demyelinating often recede again. However, permanent damage from tissue death is also possible. In the case of an intermittent course, the therapy starts with the administration of cortisone. In some cases, however, the affected patient does not respond to the cortisone.
The treatment thus differs from that of multiple sclerosis, where special immunomodulators are mainly used. Long-term therapy for the disease is based on the administration of immunosuppressors, for example the active ingredient azathioprine.
Studies indicate that the antibody rituximab could also be effective in treating neuromyelitis optica. In addition to cortisone, relapses in neuromyelitis optica can also be treated using plasmapheresis.
You can find your medication here
➔ Medicines for paresthesia and circulatory disordersOutlook & forecast
The prognosis of neuromyelitis optica is favorable with early diagnosis and successful drug therapy. The prerequisite for this is that the active ingredients of the prescribed drugs are well absorbed by the organism and lead to a regression of the inflammation. Significant improvement or recovery is documented in these patients within a few weeks.
If medical assistance is not sought, the otherwise favorable prognosis worsens. The ability to see decreases continuously and can lead to permanent blindness of the person concerned. Due to the emotional burden of the complaints, the risk of secondary psychological illnesses is significantly increased. The prognosis also worsens if the disease develops into a chronic course. It can cause irreversible damage to the optic nerve. As a result, the affected person's eyesight is impaired for life.
People who already suffer from previous illnesses and therefore have a weakened immune system, also experience delay in the healing process or persistent health complaints. In these cases, psychotherapeutic support should take place, as an interplay of emotional and physical factors can often be observed. Both areas influence each other and can therefore bring about an improvement in the overall situation if appropriate support is provided. Patients who have an intermittent or recurring disease will need regular drug treatment throughout their lives.
prevention
Effective measures for the prevention of neuromyelitis optica are not yet known according to the current state of medical research. On the one hand there is uncertainty about the exact causes of the disease, on the other hand it is an autoimmune disease.
Such diseases can generally hardly be prevented. It is therefore particularly important to consult a specialist as soon as you suspect the disease or if typical symptoms appear in order to initiate adequate therapy.
Aftercare
If you have neuromyelitis optica, follow-up examinations should take place even if symptoms are no longer evident. Follow-up examinations include checking the visual field (field of vision), the visual evoked potential (VEP, also: VECP = visually evoked cortical potentials) and magnetic resonance imaging (MRI) of the brain. The visual field is examined by ophthalmologists. Both eyes are checked individually.
It is tested which area the respective eye perceives when looking straight ahead. A VEP is carried out by the neurologist and an MRI is performed in a radiological practice. A reduced reaction time in VEP can indicate a persistent or renewed inflammation in the area of the visual pathway, a circulatory disorder or degenerative processes. An MRI of the brain then provides an image.
The treating neurologist decides which of the procedures should be carried out. If there are no symptoms, a single check is usually sufficient. In some cases, an annual follow-up examination is recommended.
Based on the results of the examination, a decision is then made as to whether and in what form a new treatment is necessary. For this, it must be checked whether the optic nerve inflammation is part of another disease. Depending on the result, further restoration then takes place. There is no special drug for the follow-up treatment of neuromyelitis optica.
You can do that yourself
The disease is accompanied by a gradual deterioration of the optic nerve. Since self-help measures are not sufficient to improve eyesight, a doctor should be consulted as early as possible.
In addition, the eyes should not be exposed to excessive stress. Do not look directly into the sun or other bright light sources. This can lead to an immediate deterioration in vision. In addition, when reading or working on the screen, there should be sufficient light sources in the area so that the optic nerve is not exposed to any further overstrain. There is always the risk of irreparable damage that should be avoided.
If there are complaints in the back area, permanent relieving or poor posture is not beneficial. These can lead to irreversible impairments of the skeletal system and trigger secondary diseases. Restrictions in mobility would be the result.In the case of inflammatory symptoms in the back, pain or tension, it is essential to work with a doctor.
A stable immune system must be ensured so that the organism has sufficient defenses available for the healing process. The body's self-healing system can be supported with a vitamin-rich diet, avoidance of obesity and sufficient exercise in the fresh air.

.jpg)