Neurotrophic Keratopathy is a disease of the eye, especially its cornea (medical cornea). It is caused by damage to the very sensitive nerve tissue there, with serious consequences for the entire eye. In science, the term keratitis neuroparalytica is usually used. The ICD-10 classification is H16.2.
What is Neurotrophic Keratopathy?

© jakubstepan - stock.adobe.com
Center of the Neurotrophic Keratopathy is the cornea. It is part of the outer skin of the eye and thus at the same time the entire eyeball. Usually it is clear with a full layer of tear fluid. Their curvature ensures that the incident light is refracted and is therefore important for correct eyesight.
The cornea is traversed by a large number of nerves and is therefore one of the most sensitive structures in the body with regard to temperature, pain and touch. The nerves have their origin in the eyeball nerve (medical nervus ophthalmicus), a secondary branch of the trigeminal nerve.
If this or the individual nerves in the cornea are damaged directly, neurotrophic keratopathy can develop. However, only a few patients are affected by this. In Europe alone, it is just 0.05 percent of the total population who have been diagnosed with one of the three defined degrees of severity of the disease.
causes
The main cause of neurotrophic keratopathy is the decreased secretion of tear fluid caused by nerve damage, which normally supplies the cornea with sufficient nutrients and at the same time forms a safe protective shield. If there is a disorder in this area, degenerative changes occur.
Various degeneracies, restrictions in functionality, regression and, in severe cases, corneal ulcers (medical ulcus corneae) are possible. The wound healing of the cornea is disturbed at the same time. In almost twenty percent of all cases, the nerve damage is triggered by herpes viruses and the infections they cause.
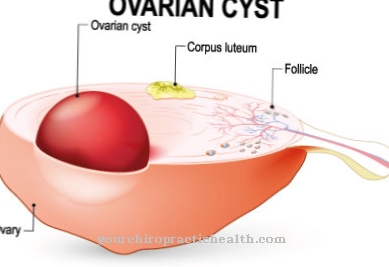
Physical injuries, chemical burns, incorrect use of contact lenses, or mistakes in surgical procedures are also possible. On the other hand, underlying diseases such as diabetes mellitus, multiple sclerosis or leprosy are less likely to be responsible for the disease. The same also applies to various tumors, cysts and abscesses. Congenital eye diseases, on the other hand, hardly play a role in the formation of neurotrophic keratopathy.
Symptoms, ailments & signs
Neurotrophic keratopathy is generally quite vague. Most of the symptoms also occur in other eye diseases and cannot be clearly assigned to neurotrophic keratopathy. The clearest sign of the disease, however, is the reduced sensitivity of the cornea.
As a result, certain stimuli, such as touch or temperature differences, are hardly or not at all perceived by the patient. Those affected are therefore painless even in a severe stage of the disease. Neurotrophic keratopathy becomes visible through a pronounced clouding of the otherwise clear cornea.
In addition, a noticeable reddening of the eye and a reduced blink reflex can be seen. The patient's visual acuity can still fluctuate a little in the beginning. However, the more severe the disease progresses, the weaker the visual acuity of the affected eye.
Diagnosis & course of disease
In order to diagnose neurotrophic keratopathy, a thorough anamnesis should be carried out to research the cause. On the other hand, various medical examinations, such as a sensitivity test of the cornea or a function test of the tear film, are necessary. Due to the ambiguous symptoms, particularly careful testing is mandatory in order to prevent the disease from progressing as early as possible.
If left untreated, neurotrophic keratopathy can lead to corneal ulcers, loss or at least perforation of the cornea, or what is known as aseptic necrosis. Even if it is mild, it can cause accompanying changes in the conjunctiva and at a later stage pose a risk to the entire eye.
Complications
Neurotrophic keratopathy can lead to serious complications, especially in the third stage. Since the disease is not accompanied by pain, it is often recognized too late. Occasional fluctuations in visual acuity should therefore give rise to urgent medical advice in order to avoid complete destruction of the cornea. As part of the disease, there is always the risk of bacterial superinfection.
Besides viruses, the cornea is also attacked by bacteria and fungi. As a result, a so-called ulcus corneae can develop. Ulcus corneae is a corneal ulcer, which is characterized by painful and constantly watering eyes. The secretion that flows out may even contain pus, which indicates a bacterial infection. The eye is then inflamed and very sensitive to light.
Sometimes an eyelid cramp is observed, which is noticeable by excessive blinking on both sides during fatigue, emotional tension or bright light stimuli. The eyelid cramp can even cause the eyes to close for several hours. Overall, the visual acuity deteriorates with ulcus corneae. In severe cases, the cornea can be perforated. This poses a great threat to the eye and can lead to blindness. In addition to extensive antibiotic treatment, surgical intervention is necessary to prevent this serious complication.
When should you go to the doctor?
If visual disturbances, eye pain, and other known signs of neurotrophic keratopathy are noticed, a doctor is advised. If physical complaints occur without a clear cause being found, a clarification discussion with the family doctor is necessary. This is especially true with increasing eye discomfort or an increased sensitivity of the cornea. Repeated tears and swelling around the eyes are best cleared up immediately. The doctor can diagnose neurotrophic keratopathy and, if necessary, start treatment directly or refer the patient to a specialist.
The risk groups include people who have recently had a viral infection or ocular herpes zoster. Victims of physical injuries and chemical burns should also consult their doctor if they have mentioned symptoms. Anyone who suffers from the symptoms mentioned after a surgical or neurosurgical procedure should inform the responsible doctor. The same applies if symptoms occur after using contact lenses or tropical medicines. Diabetes, leprosy and multiple sclerosis patients should inform the responsible health professional about unusual symptoms in the eye area. Neurotrophic keratopathy is treated by an ophthalmologist or an internist. Seriously ill patients must be treated in a specialist clinic.
Treatment & Therapy
The treatment of neurotrophic keratopathy is still difficult and depends entirely on the individual characteristics of the patient. Optimal success can only rarely be achieved with the current therapies and so the main focus is on preventing the disease from spreading. This is mainly done by giving unpreserved tear replacement fluid to supply the cornea with sufficient nutrients.
In some cases, special eye drops made from the patient's blood serum are recommended. Therapeutic contact lenses can be worn to protect the cornea. Alternatively, there is the option of performing an operation to completely or partially close the eyelid gap or sewing an amniotic graft onto the cornea.
Parallel inflammations are generally treated with a special eye ointment or gel. Existing ulcers are often reduced by the administration of antibiotics. You can choose either the tablet form or local use.
If neurotrophic keratopathy is based on a certain underlying disease, a two-pronged therapy is necessary for the patient. Here it is necessary to stop the spread of the corneal damage and at the same time fight the actual cause. This applies, for example, to diabetes mellitus or multiple sclerosis as well as to the removal of tumors or cysts that trigger it.
You can find your medication here
➔ Medicines for eye infectionsOutlook & forecast
The prognosis for patients with neurotrophic keratopathy depends on the cause. In the event of a chemical burn, the damage is usually irreversible and healing is no longer possible. If there is a viral disease, medication must be used to prevent the virus from spreading and at the same time to kill it. Normally, the person concerned suffers from further complaints, which then usually recede completely.
Surgery is often required for cysts and abscesses to enable improvement. If the person concerned suffers from a tumor disease, the further course of the disease is shaped by the progress of the disease and the treatment options. In an advanced stage of the disease, the patient threatens premature death despite all efforts. If the neurotrophic keratopathy is triggered by the incorrect use of visual aids, a change in the use of the auxiliary devices is necessary. Otherwise, an increase in complaints is possible.
Overall, the treatment options for those affected usually lead to an alleviation of existing irregularities, but not always to a complete cure. The best possible success is achieved if a diagnosis and therapy start are made at the first health irregularities. Doctors often try to curb the progression of the disease and minimize the risk of secondary health problems. Without treatment, the symptoms increase.
prevention
The most important preventive measure for neurotrophic keratopathy is to protect the cornea and avoid injury. Attention should be paid to the proper use of contact lenses, the wearing of protective goggles in dangerous situations and the risks of voluntary laser treatment for ametropia. Careful hygiene and regular check-ups by the ophthalmologist are also important.
Aftercare
Neurotrophic keratopathy lasts for a lifetime, since the damage caused to the nerves is usually not curable. Therapy adapted to the stage of the disease is therefore usually part of everyday life for the patient. Due to the lack of sensitivity of the cornea, exacerbations of neurotrophic keratopathy are not always noticed.
Constant checks by an expert ophthalmologist are therefore mandatory. This can record and document the course of the disease by measuring the eyesight. If corneal injuries occur repeatedly, further therapeutic measures may be necessary. These protect the cornea and prevent the occurrence of tumors.
Since the cornea is no longer as resistant to neurotrophic keratopathy, it should be given special protection in the future. This includes wearing protective goggles for dangerous activities, avoiding bright light sources and using contact lenses appropriately. Patients should also ensure adequate rest periods between heavy loads on the eye.
This includes working in low brightness or constantly looking at a screen. Drink logs help to control and optimize daily fluid intake. This ensures that the eye is supplied with sufficient tear fluid. All of these preventive measures can have a positive effect on the course of the disease, but they do not replace regular visits to the doctor.
You can do that yourself
In everyday life, the eye should not be exposed to bright light sources. You should avoid looking directly into the sun or into the bright spotlights of a lamp. The process can lead to injuries to the eye and exacerbate the existing symptoms. In addition, when reading or working on the screen, care should be taken that the surroundings do not become too dark. This fact also leads to an overload of the optic nerve and discomfort.
If the person concerned notices that the eye has been subjected to excessive strain, breaks must be taken immediately. The eye should be given the opportunity to regenerate during rest phases. There should be no activities such as reading, writing or watching television.
To ensure that the eye is always supplied with a sufficient amount of tear fluid, the daily intake of beverages must be monitored and, if necessary, optimized. As soon as a dry eye is noticed, the person concerned should react. Consultation with a doctor is always necessary in the event of injuries to the eye. A control visit should also be initiated if there are fluctuations in vision.
The self-help measures are not sufficient to adequately determine whether defects in the sensitive area have occurred. Anomalies and irregularities can only be identified and documented by precisely measuring eyesight.



.jpg)






.jpg)



.jpg)










.jpg)
