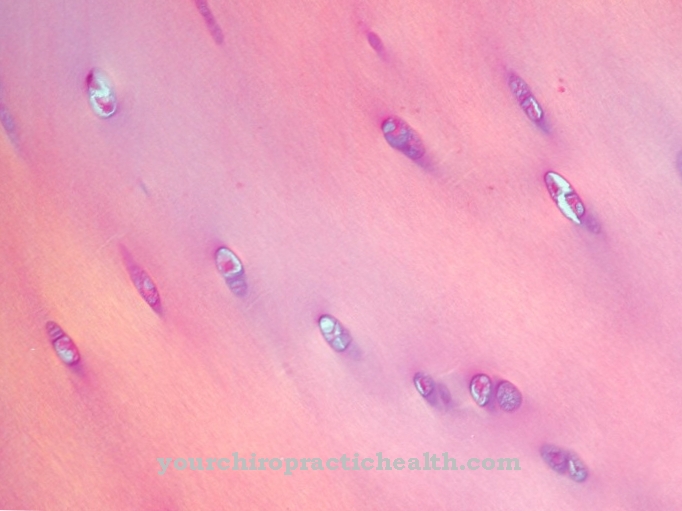
Osler nodules are changes in the skin on the fingers and toes. They are small lumps that cause pain. They often appear in hundreds of them side by side.
What are Osler nodules?

© esoxx - stock.adobe.com
The Osler nodules were named after the Canadian doctor Sir William Osler. As the first author, he first described the abnormalities of the skin changes in his patients around 1900. The nodules are also called Osler spots because they look like patches of skin. The nodules are painful skin changes.
The pain arises as soon as pressure is applied to the affected area of the skin. The Osler nodules are about the size of a pinhead to a pea. A peculiarity of the nodules is that they usually appear in numbers of several hundred at the same time. Their color is bluish-red. The nodules are diagnosed on the fingers and toes.
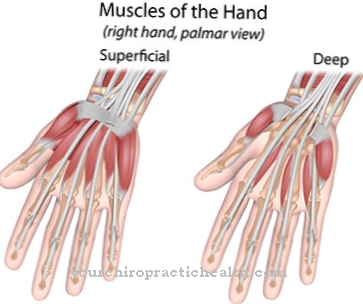
In addition, they can arise in the palm of the hand in the ball of the thumb or little finger. The skin changes are caused by bleeding into the dermis. This is the dermis, which is under the top layer of skin, the epidermis. Osler nodules are a common side effect of bacterial cardiac inflammation.
In patients, skin areas of different sizes that are affected are often found on several fingers at the same time. It is characteristic that there is often a white area of skin in the middle of the nodular spots. When treatment begins, the nodules usually disappear after a few days.
causes
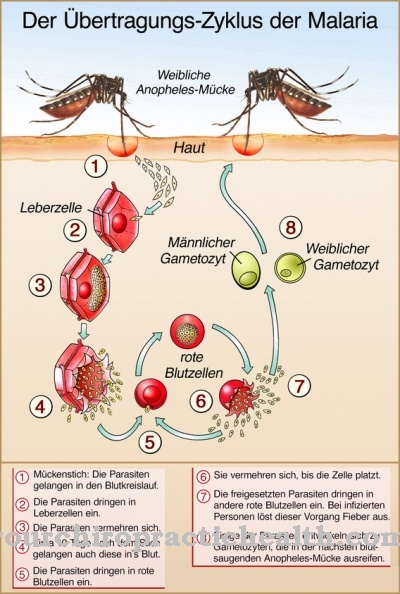
Osler nodules are caused by an embolism or inflammation due to immune complex deposition in small arteries. For both reasons, tiny drops of blood clog the veins. This causes the bleeding in the second layer of skin.
The most common cause of Osler nodules is bacterial endocarditis. Untreated infectious endocarditis can be fatal. It is an inflammation of the inner skin of the heart. The Osler nodules are a factorial and therefore not a compulsory symptom of endocarditis. In addition, the pods appear in some other clinical pictures.
They include systemic lupus erythematosus, disseminated gonococcal infection and an embolism in a septic catheter. Systemic lupus erythematosus is an autoimmune disease of the skin and the vascular connective tissue of the organs. Lupus erythematosus is assigned to inflammatory rheumatism.
Disseminated gonococcal infection is a special form of gonorrhea. In one to three percent of untreated gonorrhea, the disease turns into a disseminated gonococcal infection. The patient suffers from attacks of fever, complains of joint problems and skin changes in the form of painful nodules.
Symptoms, ailments & signs
Osler nodules are primarily noticeable as abnormal skin changes. The characteristic nodules mainly develop on the toes and fingers. There it comes to painful growths that significantly restrict the freedom of movement of the hand or foot. The nodules range in size from a few millimeters to a few centimeters, increasing in size and becoming increasingly hardened during the disease.
As the nodules heal, the skin in the affected area flakes heavily. This usually accompanies itching and redness. Depending on the cause, other symptoms can occur with Osler nodules. If the skin changes are caused by infectious endocarditis, fever, chills and palpitations occur, among other things.
Anemia and weight loss can also occur. If a heart defect is the cause, it can lead to cardiac arrhythmias up to and including a heart attack. The same applies if the Osler nodules are caused by an autoimmune skin disease. If inflammatory rheumatism is the trigger, further movement disorders occur.
At the same time, there may be pain in the limbs, symptoms of paralysis and the typical inflammatory reactions. The Osler nodules themselves subside as soon as the underlying disease has been treated. In the absence of treatment, the growths multiply and the accompanying symptoms become stronger.
Diagnosis & course of disease
The diagnosis of Osler nodules is made by a dermatologist. The Osler nodules are to be distinguished from Janeway lesions. These look very similar to the nodules, but are completely painless for the patient. In addition, they differ from the skin changes in Osler's disease.
Here they are innate and genetic changes. The diseased areas also affect the mucous membranes, the gastrointestinal tract and skin areas on the face. The Osler nodules affect skin changes on the fingertips and toes. In addition, they can occur in the palms of the hands or on the arms or legs.
However, they cannot be found inside the body. Their high number and group-like appearance are characteristic. Further examinations are not required for Osler nodules and are not recommended. The diagnosis is made after the anamnesis, visual inspection and pressure test. The latter should be associated with pain in the patient.
A typical course of the disease in Osler nodules is to be classified as remitting. Even without a doctor's visit or an explicit diagnosis, symptoms can decrease after a few days. This happens especially when the primary disease is recognized and treated. If this does not happen, the Osler nodules can be expected to recur.
Complications
In most cases, the Osler nodules have various changes and discomforts on the skin. The nodules themselves mainly occur on the toes or fingers and can therefore lead to significant restrictions and discomfort in the everyday life of the person concerned. The patient's quality of life is significantly restricted and reduced due to the Osler nodules.
The nodules themselves are painful, so that most people can no longer easily do many things with their fingers. This can also lead to psychological complaints or even depression if the disease is not treated properly. In many cases, a simple diagnosis of Osler's nodules is not possible. The treatment itself usually runs without complications and is supported with the help of antibiotics.
Success is achieved relatively quickly. However, the skin flakes relatively heavily during the treatment. Many patients also suffer from inferiority complexes or from a significantly reduced self-esteem. As a rule, protecting the hands and feet also has a very positive effect on the Osler nodules. The life expectancy of the patient is not reduced with this disease.
When should you go to the doctor?
Reddish lumps on the toes and fingers, bleeding under the nails, and other signs of Osler nodules should be cleared up quickly. If the skin changes and pain do not go away by themselves, medical advice is required. The affected persons should consult their family doctor, who can often identify the Osler nodules by visual diagnosis. If necessary, further diagnostic measures must be initiated, for example a biopsy and imaging procedures, in order to be able to determine the disease beyond doubt. People who already have endocarditis must tell their doctor about the nodules.
If the symptoms arise after a skin infection or other skin disease, medical advice is also required. Patients can visit the dermatologist or an internal medicine specialist. The treatment is usually medicated and can be carried out at home by those affected. Close contact with the doctor must be maintained during therapy.
If side effects or other complications occur, the doctor must be informed. The Osler nodules should subside quickly with early treatment. Further visits to the doctor are usually not necessary. However, the weakened skin is prone to further infections, which is why the dermatologist should be consulted regularly at least in the first few weeks after recovery.
Treatment & Therapy
The treatment of Osler nodules depends on the cause. As long as this has not been finally clarified, the painful skin changes will recur. If you have endocarditis, we recommend working with an internist. Systemic lupus erythematosus is treated with an ointment or cortisone, depending on the stage.
However, the ointment is not applied directly to the skin areas of the Osler nodules, as the ingredients are tailored to the rheumatic complaints. Disseminated gonococcal infection is treated with penicillin or antibiotics, depending on the pathogen. Provided that the cause of the nodules has been found and treatment measures have been successfully initiated, the Osler nodules usually heal without further medical intervention.
In the further healing process, the skin gradually sheds the topmost layer of skin by itself. This process lasts for a few days and is usually painless for the patient. During this time you should avoid scratching or deliberately rubbing the surface of the skin.
Skin-irritating or chemical products, for example from household cleaning, should not come into contact with the skin without protection. Skin care products without the addition of alcohol can also be used as support if desired. Activities that put pressure on the affected areas of the skin should be avoided.
It is advisable to protect your hands, arms and legs for a few days. The wearing of rubber gloves is only recommended when performing strenuous activities.
You can find your medication here
➔ Medicines against redness and eczemaOutlook & forecast
The development of Osler nodules - also known as Osler's disease - is based on a genetic disease. This already includes the statement that a cure is not feasible with such vascular changes. For most genetic diseases, only the sequelae and symptoms can be alleviated. With close monitoring of those affected and symptomatic therapy, Osler's disease patients can experience a good quality of life.
For Osler's disease, the symptomatic therapeutic approaches guarantee an almost normal life for many of those affected. What should be avoided with Osler nodules is diving. Air embolism can occur when using compressed air cylinders. In order to keep the other prognosis in the positive range, regular checks by the attending physician are advisable. Certain medical conditions or pregnancy can lead to serious complications if Osler nodules are present. Increased age can also worsen the prognosis.
If internal organs are involved in complications, the prognosis worsens. Age and pregnancy can aggravate pulmonary arterial-venous malformations. It causes bleeding. Therefore, the prognosis varies from patient to patient. The course of the disease can also change in the course of life. While some patients with Osler's nodules have only minor symptoms, others affected experience life-threatening conditions due to a change in the course of the disease.
prevention
Preventive measures are not recommended for Oslo nodules. Since they are side effects and side effects of some other diseases, intervention measures are possible with them. For example, hygiene should be observed when laying a catheter. Gonorrhea should also be treated immediately.
Aftercare
As a rule, those affected with an Osler nodule have only a few or only limited follow-up measures available. However, these are not always necessary, so that the disease does not always have to be treated directly. An early diagnosis has a positive effect on the further course of the disease and can also prevent further complications or complaints from occurring.
The disease can usually be treated relatively well with the help of various drugs. The person concerned should always follow the doctor's instructions and take the medication regularly and in the correct dosage. When taking antibiotics, it should also be noted that they should not be taken with alcohol.
If there are severe side effects, a doctor should also be consulted. Regular checks by a doctor are very useful during treatment. In general, the skin of Osler's nodules should be protected particularly well, avoiding contact with the excitatory substances. The condition does not reduce the person's life expectancy.
You can do that yourself
Depending on the underlying cause of the Osler nodules and the treatment steps that have already been taken, the patient can support recovery through various self-help measures.
Above all, strict personal hygiene has proven itself. The affected area must be treated with suitable preparations in order to avoid the development of dandruff and other skin changes. At the same time, the patient should take it easy. In order to avoid serious complications, the affected area must not be exposed to any further stimuli, especially after an operation. Hands, arms and legs must always be spared, preferably by wearing special gloves and getting enough bed rest.
In the further recovery process, the Osler nodules should not come into contact with fabric and should not be rubbed under any circumstances. Products that irritate the skin should be avoided for the first few days to weeks. This applies not only to personal hygiene, but also to household cleaning and occupational activities. The responsible doctor can answer which measures are indicated in detail. Since Osler nodules can appear in very different forms and numbers, any self-help measures should only be used after a comprehensive consultation with a dermatologist.



.jpg)

.jpg)



.jpg)


.jpg)






.jpg)
