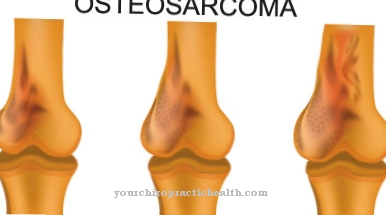
The doctor then speaks of an inflammation of the bone (Osteitis), if there is an infection that - in very many cases - contains malignant microorganisms. Surgery or open fractures (breaks) increase the risk of one Inflammation of the bones. In very many cases, radical operations are the only treatment option if the patient is affected by osteitis.
What is an osteitis?

© Pixel-Shot - stock.adobe.com
Under one Osteitis respectively Inflammation of the bones the doctor describes a special infection that mainly affects the bones. In the Osteitis, the Havers or Volkmann canals can be affected. If the Haversian canal is infected with pathogens, it is an infection in the longitudinal directions of the supply lines of the bone. The nerves and capillaries run in these canals.
If the pathogen is present in the Volkmann canals, it is an infection in the transverse directions of the bone structures. In many cases, however, osteitis occurs in combination with inflammation of the bone marrow. Due to the fact that osteitis and bone marrow inflammation (osteomyelitis) have similar clinical pictures, medical professionals often use the terms ostitis, osteitis and Osteomyelitis as a synonym.
causes
The osteitis develops due to an infection. Foci of infection that has already caught fire in the body rarely spread to the bones. In most cases, an osteitis occurs as part of an open fracture. The pathogens enter through the open wound, attack the bones and cause inflammation. Even surgery increases the risk of osteitis. For example, when germs - due to non-sterile instruments - get into the wound and directly onto the bone.
Sometimes viruses and fungi can cause bone inflammation; in almost all cases, however, bacteria are responsible for osteitis. Streptococci in particular play an important role. Bacteria that occur as part of a nosocomial infection can also trigger osteitis. These are mainly classic infections that occur in nursing homes and hospitals. It is mainly multi-resistant germs that cannot be fought by antibiotics. Sometimes the pathogens also include strains of Staphylococcus aureus; that tribe is the main cause of an Osteitis.
Symptoms, ailments & signs
Classic symptoms are redness and swelling of the affected area. The patient complains of bone pain, has a high body temperature, or has a fever. In many cases, those affected are knocked out and report pain in their limbs and joints, although fractures can occur later in the disease. If the osteitis is not or insufficiently treated, pus can leak out.
Diagnosis & course of disease
Osteitis is noticeable through five classic symptoms of inflammation. Those appear together. These are redness, heat, pain, swelling and functional restrictions. If there are open wounds or fistulas, pus formation can be observed. The doctor recognizes the osteitis from the blood count. During blood tests, the doctor not only finds a strong inflammatory reaction, but also a significantly increased leukocyte value.
Magnetic resonance imaging provides information about whether bone changes have already occurred. Sometimes necrotic processes can also have occurred. This means that the bone substance dies. If there is osteitis, only radical operations can promise success. Those are risky, but cannot be postponed or prevented. Depending on the extent of the osteitis, permanent damage or disabilities can occur.
Complications
In most cases, osteitis results in very severe swelling of the affected area of the body. After the fracture of the bones, the patients usually suffer from very severe pain and restricted mobility. The person affected may then be dependent on the help of other people in their everyday life.
The osteitis also leads to a high fever and general fatigue in the patient. Resilience also drops significantly and pain occurs in the extremities and joints. The patient's quality of life is generally significantly reduced by the osteitis. Complications usually arise if treatment is not given. The inflammation can also spread to other areas of the body and possibly also penetrate outside.
In the worst case, blood poisoning can also occur, which can be fatal for the person concerned. The treatment of osteitis is usually carried out through surgical interventions and with the help of antibiotics. As a rule, the disease progresses positively without complications. The life expectancy of the person affected is usually not influenced by the Osteitis.
When should you go to the doctor?
If you have bone or joint pain, you should see a doctor. Osteitis is manifested by discomfort in the area of the bones, which quickly become stronger and spread as the disease progresses. If the symptoms mentioned appear, the family doctor must be consulted. This can make a diagnosis using a scintigraphy and inform the patient about the next steps. People who already have a bone disease are particularly at risk. There is also an increased risk of disease for older people and patients with genetic predispositions such as malformations.
Likewise, people who suffer from bone cancer or who can no longer move because of an existing condition have an increased risk of complications and should see their doctor immediately if the described bone pain or joint dysfunction is noticed. Osteitis is treated as an inpatient in a specialist clinic. The patient should go to regular follow-up care after the operation and also consult the doctor if there are unusual symptoms.
Therapy & Treatment
Due to the fact that osteitis is a bacterial infection, antibiotics must be prescribed. In many cases, oral medication is insufficient; Infusion drugs are often prescribed, but they do not lead to the desired success. For this reason, the doctor - in almost all cases - has to operate and peel off the affected area of the bone.
The doctor focuses on the inflamed or already necrotic part of the bone. If stabilizing measures in the form of screws or nails have been taken as a result of fracture treatment, the doctor must remove those instruments. However, the break point must still be fixed; for this new or different instruments are used. Disinfecting rinses also take place during the operation. The pathogens should be completely removed.
Chains or tamponades soaked with antibiotics remain in the surgical wound. In addition, a drain is inserted so that the purulent secretions can be drained away. The doctor can sometimes leave the surgical wound open if there is a risk of having to perform another operation. Because the operation does not always bring the desired success and healing of the osteitis with it. Because of this, a second surgery may be required.
Even if the healing process has already started and there is a suspicion that there are still foci of inflammation, a second operation can be performed. Due to the fact that the interventions have caused a loss of substance, this must be compensated again. Thus the patient has to work on restoring his mobility. In the absence of or inadequately performed rehabilitation, a disability can sometimes impair mobility.
Outlook & forecast
The prognosis of the Osteitis depends on various factors. This includes the age of the person affected, the type of inflammation and the type of bacteria causing it. The strength of the immune system also plays an important role.
The outlook for osteitis is positive if there is acute bone marrow inflammation.Even in the case of bone inflammation, healing can be achieved in most cases without permanent impairment. The basic requirement, however, is an early diagnosis and appropriate expert treatment.
The prognosis is less favorable in the case of chronic osteitis. Chronic bone inflammation primarily affects adult patients. In contrast, the chances of recovery for children are rated as more favorable. However, growth disorders can sometimes be expected in children if the growth plates are affected by the inflammation. The growth plates in children are still made up of cartilage. The cartilage constantly creates new bone substance for growth. However, if this process is disturbed, there is a risk of short stature. Depending on the location of the inflammation focus, arms or legs can be shortened.
The chronic course of the Osteitis often lasts for several years. It can also occur again. Relapse can occur even years after treatment. Curbing the inflammation through surgery usually has a positive effect on the course.
prevention
Osteitis can only be prevented to a limited extent by the person affected; rather, the hospital must - within the framework of hygiene - ensure that osteitis is prevented. If a bone inflammation is suspected, a doctor must be contacted immediately.
Aftercare
In the case of osteitis, follow-up measures are usually significantly limited. For this reason, those affected with this disease should consult a doctor very early to prevent further complications or further complaints for the person concerned, which could negatively affect the patient's quality of life. An early diagnosis usually has a very positive effect on the further course of the disease.
In most cases of osteitis disease, another surgical procedure is necessary. After this procedure, the person affected should take it easy and rest, while keeping bed rest. The wound should be particularly well protected so that there are no further infections and other complaints.
Regular checks are also very important after the person concerned has been discharged. Usually, osteitis does not reduce the patient's life expectancy if detected and treated in a timely manner. Further follow-up measures are usually not available to the affected person and are not necessary. In general, however, a high standard of hygiene should be observed.
You can do that yourself
Once the diagnosis of osteitis has been confirmed, the affected patient should reliably take the medication (antibiotics) prescribed for him or have them infused according to the doctor's instructions. The doctor may need to operate to prevent sepsis. Despite all therapeutic measures, other sources of inflammation may be active in the body. It is therefore advisable for the patient to also take action against the inflammation.
In orthomolecular medicine, the intake of the mineral zinc and vitamins C and E is recommended for inflammation, while phytotherapists would recommend herbal remedies such as coneflower, chamomile or linden blossom. A naturopathic doctor can give specific recommendations here. If the inflamed areas are still swollen, they should be cooled. Cooling cushions or so-called coolpads, which are available in pharmacies, are suitable for this. They should be stored in the freezer compartment of the refrigerator and, if necessary, wrapped with a towel and placed on top. Under no circumstances should the cooling pad come directly onto the skin, as this can cause cold burns.
During this time it is important to strengthen the patient's immune system. This includes a healthy diet rich in vitamins and minerals as well as regular sleep. At the same time, the patient should refrain from using drugs such as nicotine, coffee and alcohol. Daily exercise in the fresh air also supports the immune system.