The Osteoclasts are giant cells that are responsible for bone breakdown and demineralization. Their activity is regulated by various substances, such as parathyroid hormone. Too much or too little osteoclast activity has serious effects on skeletal health.
What are osteoclasts?
Every seven years the human being receives a completely new skeleton. Human bones adapt to loads and are constantly being remodeled. They are renewed after microfractures and fractures. The defective bone mass is removed and new bone mass is built up.
The so-called osteoblasts are responsible for the construction work. These are immature bone cells that later mature into osteocytes. The breakdown work in the bone metabolism is not carried out by the osteoblasts, but by the osteoclasts. These bone cells arise from precursor cells from the bone marrow and migrate into the skeletal system as required. Their work involves two different mechanisms: the demineralization of the bone substance and the actual breakdown of the bone.
By their work, osteoclasts slow down bone growth and prevent excessive growth processes and growths. They communicate with the osteoblasts via the key substance RANKL. In addition to this communication, the hormonal cycle plays a role in their regulation. The parathyroid hormone activates the breakdown and calcitonin inactivates the osteoclast activity.
Anatomy & structure
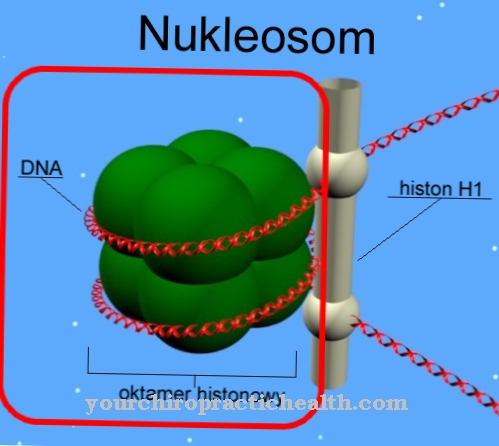
Osteoclasts are multinucleated cells and therefore belong to the so-called giant cells. They are created by the fusion of mononuclear precursor cells in the bone marrow, also known as blood stem cells.
They are part of the mononuclear phagocytic system. This means the entirety of all cells of the reticular connective tissue, some of which is part of the immune system and is responsible for the breakdown and removal of waste and foreign particles. Osteoclasts have a diameter of 30 to 100 µm and can contain over 20 cell nuclei. They sit on the surface of the bone in the Howship lacunae and move amoeboid. Your apical pole of one points to the bone. In the center lies a zone containing vesicles with a cell membrane folded like a flower. This "ruffled border" is the place for the resorption of the bone.
The periphery of the osteoclasts is intensely stained. The adhesion apparatus there allows the cells to adhere to the bone with a minimal distance of 0.3 nm. This "sealing zone" is enclosed by the cytoplasm, which is also called the "clear zone" and has only a few cell organelles, but many contractile proteins.
Function & tasks
The build-up and breakdown processes of the bone substance are ideally coordinated and are controlled by a finely regulated control circuit. The osteoclasts are stimulated to form by various factors. Above all, dexamethasone, 1,25- (OH) 2VitD3, parathyroid hormone, PTHrP, prostaglandin-E2 and cytokines act as bone resorptive. In contrast, bisphosphonates, calcitonin and estrogens have an inhibiting effect on the osteoclasts.
These factors regulate the activation of the so-called PU.1 transcription factor. It controls the conversion of the bone marrow macrophages into multinucleated osteoclasts. The substances RANKL and osteoprotegerin are also involved in activation. The hormonal control circuits use the bones as a kind of buffer to regulate the calcium balance. The bone resorptive parathyroid hormone releases calcium, for example. Calcitonin, on the other hand, stimulates the storage of calcium. The permanent build-up and breakdown of bone substance controlled in this way means that the skeletal system adapts to loads and changes. In this way, material fatigue is prevented. In the meantime, osteocytes have also been assigned a role in osteoclast regulation.
Osteocytes are trapped osteoblasts that have matured. When a bone is affected by a fracture or microfracture, the osteocytes die due to a lack of nutrients and the substances released call the osteoclasts on the scene. The work of osteoclasts consists of two mechanisms. There is a minimal gap between an osteoclast and the bone substance in which the pH value is reduced. Through this degradation, the bones become demineralized. Mineral salts are extracted. The pH value required for this is kept constant by active proton transport. The osteoclasts remove the collagenous bone matrix using proteolytic enzymes. In doing so, they phagocytize the released collagen fragments.
Diseases
When osteoclast activity falls or increases, this change can become pathological. Decomposition and reconstruction are ideally coordinated in healthy bones.
Decreased osteoclast activity can therefore cause just as much damage as increased activity. In genetic osteopetrosis, for example, there is a greatly reduced osteoclast activity. Increased osteoclast activity is characteristic of non-genetic osteoporosis, hyperparathyroidism, osteodystrophia deformans and aseptic bone necrosis. The same is true of rheumatoid arthritis, periodontitis and osteogenesis imperfecta. When the osteoclasts are more active, bone mass is broken down faster than it can be reproduced.
Those affected therefore suffer from fragile and weak bones. In hyperparathyroidism, the regulatory apparatus of bone formation itself is affected. The epithelial cells are abnormal and thus dysregulate the calcium level in the body in the form of parathyroid hormone. The reason for this is the increased secretion of the parathyroid hormone, which can be traced back to an adenoma or an enlargement of the parathyroid glands. The increased parathyroid hormone level increases bone loss. The result is severe bone pain and reduced calcium excretion in the kidneys. The amount of calcium in the blood increases and causes kidney stones.
Typical & common bone diseases
- osteoporosis
- Bone pain
- Broken bone
- Paget's disease