A Pancreatic tumor can be benign, but also malignant, with the majority of all diagnosed tumors in the pancreas being malignant. While benign tumors can be removed relatively easily, malignant tumors or pancreatic carcinomas are known for their enormous aggressiveness.
What is a pancreatic tumor?
Under a Pancreatic tumor the doctor describes tumors that have formed in the pancreas - the pancreas. The majority of the tumors that develop are malignant; as a result, the tumor attacks the area of the pancreas that produces digestive enzymes. The ducts that lie within the organ are mainly affected.
causes
The pancreatic cells, which are responsible for the production of digestive juice, begin to grow uncontrollably. As a result, a pancreatic tumor develops. Even if there are benign and malignant tumors, malignant tumors (pancreatic carcinoma) are increasing. Malignant tumors are extremely aggressive and grow and multiply incredibly quickly.
It is characterized by the formation of metastases, which subsequently also affect other organs (such as the lungs or liver). Even if the development of a pancreatic tumor is known, the doctors have not yet found an exact cause why the growth of the pancreatic cells degenerates and a pancreatic tumor forms. Sometimes it is genetic changes that ensure that healthy pancreatic cells are transformed into tumor cells.
Symptoms, ailments & signs

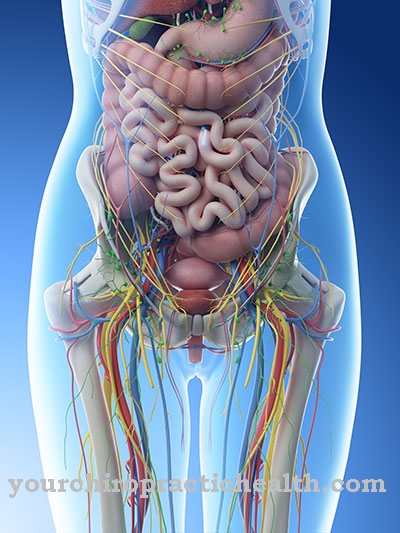
© bilderzwerg - stock.adobe.com
Increasing jaundice (jaundice) is characteristic of the pancreatic tumor; Although this usually only occurs in the advanced stage of the disease, it is considered to be a classic leading symptom of tumor disease. The patients also complain of abdominal pain, which then radiates into the back.
Pain, which is described as dull and occurs predominantly during the night, is also typical of pancreatic tumors. A bulging gallbladder (so-called Courvoisier's sign) is also an indication that a pancreatic tumor has formed. Since the pancreatic tumor blocks the inner ducts of the pancreas, the function of the glands is impaired.
So that patients also suffer from indigestion; rapid weight loss is the result. Diabetes occurs in around ten percent of all cases. Changes in skin pigmentation and thrombosis can also be the first signs of a pancreatic tumor. At an advanced stage, liver enlargements and liver function disorders are also possible; extreme emaciation and ascites appear in the terminal stages.
Diagnosis & course of disease
The doctor will perform an ultrasound scan to begin with.With the help of ultrasound, it is possible to rule out any other diseases in advance that can also trigger abdominal pain or jaundice. With the help of magnetic resonance imaging or computed tomography, the doctor can identify any tumors that have formed in the pancreas.
In a few cases a gastroscopy and an X-ray of the inner passages of the pancreas may be necessary so that a reliable diagnosis can be made. Due to improved surgical techniques, we can speak of a better healing rate today. While benign tumors can be removed easily and straightforwardly, malignant tumors in particular are extremely difficult to treat.
Pancreatic carcinoma, for example, has the worst prognosis of all carcinomas known to date. The so-called five-year survival rate is no more than 30 percent; just 20 percent of all tumors can be surgically removed after the doctor has made the diagnosis. In around 80 percent of all cases, the tumor returns - within 24 months; a second operation is only possible in very few cases.
Complications
With a pancreatic tumor there is an increased risk of complications, which is especially true for malignant tumors. Because the tumor is mostly anatomically located near the bile outflow, the bile can build up and extend to the gallbladder. As a result, there is a risk of gallbladder inflammation (cholecystitis). It is also possible that an abscess may develop in the liver.
If the inflammation of the gallbladder spreads over the whole body, life-threatening blood poisoning (sepsis) can develop. Without prompt medical treatment, this often results in the death of the patient. Sometimes a pancreatic tumor triggers a blockage in the intestine. The intestinal blockage can in turn lead to impaired metabolism or constipation.
Also, because the blood supply is reduced, there is a risk that the affected part of the intestine could become inflamed and die. A malignant pancreatic tumor often leads to metabolic disorders. It can no longer produce enough hormones and enzymes. The development of diabetes (diabetes mellitus) is also possible in the further course of the cancer.
Surgical treatment of the pancreatic tumor can also lead to complications. The different interventions are considered serious and extensive. Conceivable consequences are injuries to adjacent organs and body structures. These include above all blood vessels such as the main artery (aorta) or nerves. It is not uncommon for heavier bleeding or secondary bleeding to appear.
When should you go to the doctor?
Recurring gastrointestinal complaints, loss of weight and appetite as well as signs of type 2 diabetes mellitus indicate a pancreatic tumor. A doctor should be consulted if these symptoms occur without a clear cause. If further unusual symptoms and complaints occur, it is best to consult your family doctor or a gastroenterologist.
A pancreatic tumor manifests itself through aggressive growth and rapid metastasis, which is why an early diagnosis can be life-saving. Smokers, alcoholics and people who are overweight are particularly likely to develop pancreatic tumors. Diabetes patients as well as people with a familial accumulation of the disease also belong to the risk groups. If these factors apply or if you lead an unhealthy lifestyle with little exercise and a one-sided diet, the symptoms described should definitely be clarified by a doctor.
The family doctor, an oncologist or a gastroenterologist is responsible. Nutritionists, physiotherapists and psychologists are also consulted during treatment. Therapy always takes place under the supervision of a specialist, who must be informed of all unusual symptoms, side effects and events related to the disease. Since there is a high risk of recurrence, the patient has to go to cancer screening at regular intervals after therapy.
Therapy & Treatment
Four out of five carcinomas can no longer be treated surgically once the doctor makes the diagnosis because the patient is already at an advanced stage. Even if only isolated metastases have been diagnosed in the liver, the operation does not lead to a cure. However, if the tumor has neither caused distant metastases nor has it infiltrated larger arteries, complete removal of the tumor is possible.
However, if there is an infiltration of the veins, an intervention is also made impossible. As part of the operation, the doctor also removes the lymph nodes - even if they are not affected. Even if this variant is controversial, more and more doctors are opting for the removal of the still healthy lymph nodes.
During the surgical procedure, the doctor does not try to remove the entire organ, so that a connection with the intestine is still possible. Depending on the location, the doctor decides on a right-sided (duodenopancreatectomy), left-sided (pancreatic tail resection) or middle partial resection of the pancreas. With a partial resection on the left, the spleen is also removed in almost all cases.
Sometimes a total resection - the complete removal of the pancreas - can be the last chance for the patient to heal. Then the bile duct and stomach are connected to the intestines. For this purpose, raised loops of the small intestine are used, which are "connected" to the stomach without tension.
But if the tumor is incurable, the doctor decides on chemotherapy. Chemotherapy can also be considered useful after surgery or before surgery (if the tumor is too large and needs to be reduced in size).
Outlook & forecast
The pancreatic tumor is one of the most insidious types of cancer. According to the cancer registry of the Robert Koch Institute, the survival rate of male patients after 5 years is 6.4 percent. For women it is 7.6 percent. This means that pancreatic cancer has the lowest of all cancer survival rates. However, the prognosis of the disease depends largely on the point in time at which the diagnosis and subsequent treatment take place. The sooner the pancreatic tumor is treated accordingly, the more beneficial it will be for the course of the disease. The type of tumor also plays an important role.
Surgical removal of the pancreatic tumor is only possible in 15 to 20 percent of all patients, which also has a negative effect on the further course. The 5-year survival rate for those who have been operated on is between 22 and 37 percent. The prognosis is particularly poor if the tumor is already at an advanced stage. The 5-year survival rate is only 0.2 to 0.4 percent.
It looks better with the rarely occurring cystadenocarcinoma. This special form of pancreatic tumor has long been localized and is less aggressive. For this reason, his prognosis is more favorable. In the case of endocrine carcinomas, too, the prognosis is generally better.
In addition, a pancreatic tumor can recur. Metastasis is also possible.
prevention
Since no causes are known so far, for what reason the pancreatic cells degenerate and mutate into cancer cells, it is also not yet known which preventive measures could stop or prevent a possible tumor formation.
Aftercare
Tumor diseases require follow-up care. Many tumors form again after successful therapy. Doctors counter this life-threatening danger by closely monitoring the progress. It is no different with pancreatic tumors. Usually before the end of the initial therapy, the doctor and patient talk about follow-up care.
It should be noted that a cure is not always possible. Sometimes doctors forego treating a pancreatic tumor because it is too advanced by the time it is diagnosed. Then aftercare only has a palliative function. Those affected receive medical support so that they can live without pain for the rest of the time.
The classic aftercare takes place at least quarterly in the first and second year after the end of treatment. Then the examination rhythm expands. An annual inspection is sufficient from the fifth year of freedom from complaints. Follow-up care is carried out either in a clinic or by a doctor in private practice.
Content-related points are a symptom-related conversation and a physical examination. A doctor can view the inside of the abdomen using endoscopic echography. Computed tomography is also common. Because of the low survival rate with a pancreatic tumor, questions about life also play a role that should not be underestimated. Psychotherapy can be prescribed if necessary.
You can do that yourself
Patients with a pancreatic tumor can support themselves and their organism through a healthy lifestyle. With a balanced diet and the supply of vitamins, nutrients and trace elements, the immune system is strengthened and well-being improved.
The body needs sufficient sleep and high quality rest periods for good regeneration. Sleep hygiene should therefore be checked and adapted to the needs of the patient. The bed utensils, the fresh air supply and possible environmental influences must be checked and optimized.
Relaxation techniques and cognitive training help to build an inner balance. The patient can use these procedures and methods independently or with the help of professional support. Hustle and bustle, stress or excitement have a negative impact on health and weaken the patient. Sufficient exercise in the fresh air, leisure activities and discussions with relatives or other affected persons are perceived as beneficial and stabilizing.
The patient's focus should be on improving their wellbeing. A positive outlook on life and laughter strengthen those affected despite all adversities. An exchange with other sick people in self-help groups or internet forums can lead to new insights. Tips and hints for dealing well with the disease in everyday life help you cope with all examinations and complaints.

.jpg)

.jpg)




















