Parathyroid hormone or. Parathyrin is formed in the parathyroid glands. The hormone plays an important role in regulating the calcium and phosphate balance.
What is the parathyroid hormone?
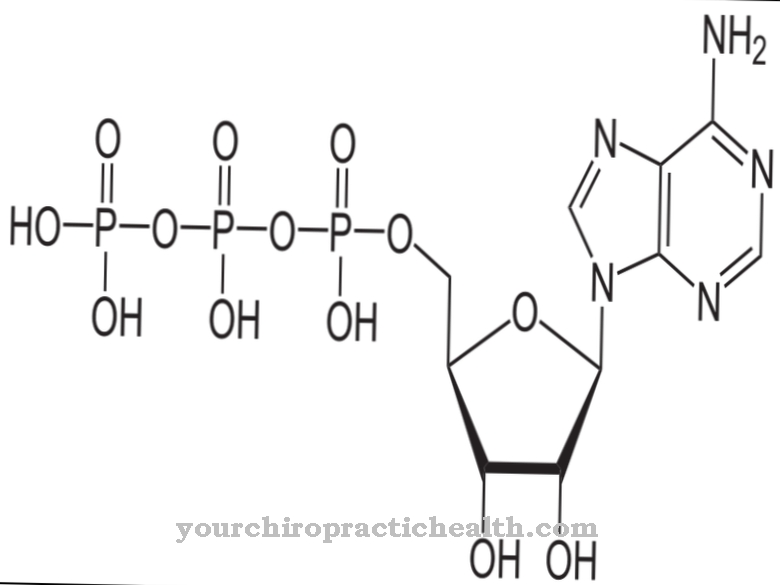
Parathyroid hormone (parathyrin, PTH) is a linear polypeptide hormone formed by the parathyroid glands (glandulae parathyreoideae, epithelial bodies), which consists of a total of 84 amino acids.
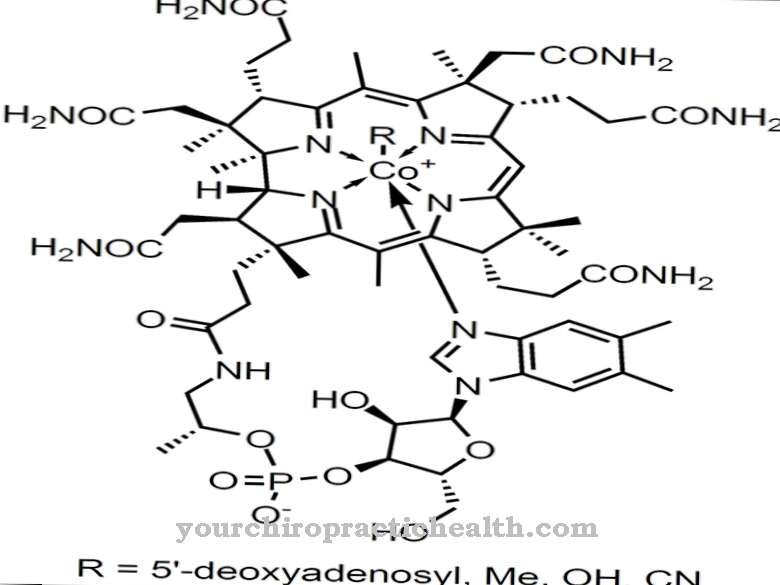
In interaction with vitamin D and its direct antagonist, calcitonin, formed in the thyroid gland, the hormone regulates the calcium and phosphate balance of the human body. In a healthy state, the reference value is around 11 to 67 ng / l in the blood.
Production, Education & Manufacturing
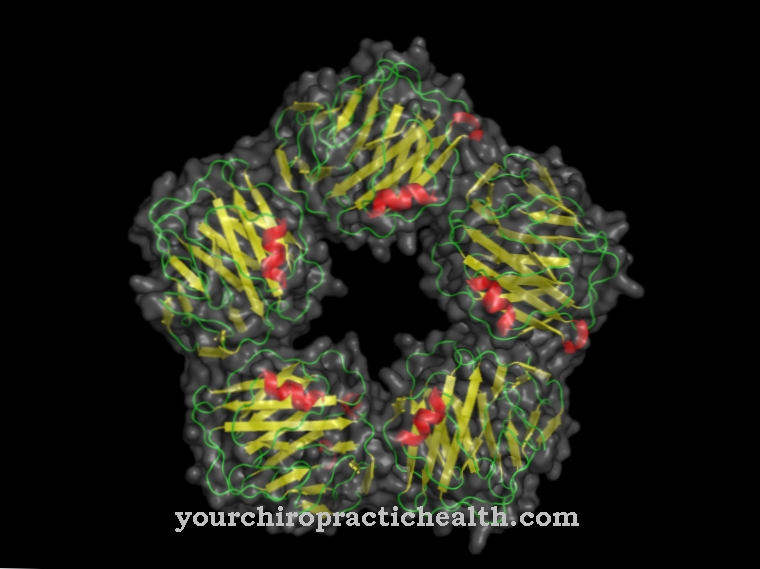
Parathyroid hormone is produced and secreted (released) by the parathyroid glands. Parathyroid glands are four small, approximately lentil-sized glands that lie in pairs on the left and right of the thyroid gland.
The peptide hormone is synthesized in the main hormone-producing cells of the epithelial corpuscles and released directly into the blood due to the lack of independent ducts (endocrine secretion). The hormone is initially formed as a precursor (prepro-hormone) consisting of 115 amino acids on the membrane-bound ribosomes. Ribosomes are RNA-rich particles on which protein synthesis takes place in the cells.
The amino terminal sequence is then cotranslational, i.e. H. during the translation of mRNA into the amino acid sequence. Another preliminary stage is created from 90 amino acids (pro-parathyroid hormone), which is processed in the Golgi apparatus (protein-modifying cell organelle) to form the finished parathyroid hormone.
Function, effect & properties
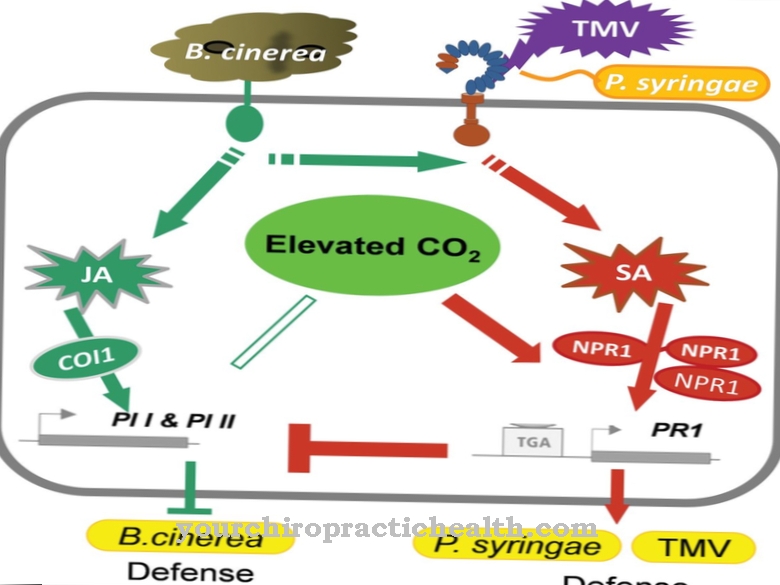
Parathyroid hormone, together with vitamin D (calcitriol) and the thyroid hormone calcitonin, regulate the calcium and phosphate levels in the blood. With the help of specific receptors on the membrane of the parathyroid cells (so-called G-protein-coupled calcium receptors), the calcium level in the blood is determined.
A decrease in the blood calcium concentration stimulates the formation and release of parathyroid hormone in the parathyroid glands, while an increased blood calcium inhibits secretion (negative feedback). Correspondingly, for example, hypocalcemia (low calcium level) forms the stimulus for the release of parathyroid hormone. The direct and indirect effects of the hormone cause adenylate cyclase (enzyme) in the bones and kidneys to stimulate the unbound, free calcium concentration in the blood.
The osteoclasts of the bones and the reabsorption of calcium in the kidneys (reduced excretion via the kidneys with urine) are directly stimulated. In addition, the phosphate concentration in the blood is reduced by increased excretion via the kidneys (inhibited reabsorption). In order to prevent demineralization of the bone, the vitamin D or calcitriol synthesis is stimulated in parallel via the phosphate level (hypophosphataemia) that has fallen in this way.
Calcitriol promotes bone remineralization by increasing calcium absorption in the small intestine. At the same time, the resulting increased calcium concentration in the blood inhibits the release of parathyroid hormones. Calcitonin fulfills an analogous function. It is released when the calcium level rises and promotes the incorporation of calcium into the bones while at the same time inhibiting osteoclast activity.
Permanent stimulation of the osteoclasts results in a gradual loss of bone mass. Therefore, for example, secondary hyperparathyroidism (overproduction of parathyroid hormone) is associated with old age osteoporosis. A fragment of the parathyroid hormone (made up of amino acids 1 to 34) is used therapeutically as a drug that stimulates bone formation.
Illnesses, ailments & disorders
In general, impairments of the parathyroid hormone metabolism are divided into so-called hyperparathyroidisms (overfunction of the parathyroid glands) and hypoparathyroidisms (underfunction of the parathyroid glands). In hyperparathyroidism, more parathyroid hormone is formed and secreted.
The concentration of hormones in the blood is increased. If the hyperfunction can be traced back to an impairment of the parathyroid glands themselves, primary hyperparathyroidism is present. This is usually caused by benign (hormone-producing parathyroid adenomas), in very rare cases by malignant tumors (parathyroid carcinomas).
In addition, hyperfunction of the parathyroid glands in connection with kidney, liver or intestinal diseases as well as a vitamin D or. Calcium deficiency occur (secondary hyperparathyroidism). A lack of vitamin D or calcium leads to a reduced blood calcium level, which in turn stimulates the parathyroid hormone synthesis in the parathyroid glands. With a long-term low calcium level, which can also manifest itself as a result of kidney insufficiency (kidney weakness), the parathyroid glands permanently synthesize more parathyroid hormone.
In the long term, this overproduction can lead to parathyroid hyperplasia (overgrowth of tissue in the parathyroid glands), which in turn is associated with manifest, primary hyperparathyroidism. In hypoparathyroidism, on the other hand, there is a reduced production and release of the parathyroid hormone and the parathyroid hormone concentration in the blood is reduced. If the parathyroid glands do not react with increased parathyroid hormone release despite a low calcium concentration, this can usually be attributed to a malfunction of the parathyroid glands (primary hypoparathyroidism).
Primary hypoparathyroidism is often caused by autoimmune diseases (including sarcoid) or partial removal of tissue from the parathyroid glands (removal of the epithelial cells or parathyroidectomy). In some cases, the parathyroid glands are also injured during surgery on the thyroid gland.
Progressive (advanced) tumors as well as an overactive thyroid can cause hypercalcemia (permanently elevated calcium level), which in turn is associated with a reduced parathyroid hormone concentration. An overdose of vitamin D also leads to a reduced release of parathyroid hormone into the blood.

.jpg)






.jpg)



.jpg)










.jpg)
