Parkinson's or Parkinson's disease is a previously incurable disease of the brain. Typical signs are a visible and severe deterioration in mobility and motor skills. A strong tremor is also noticeable. Parkinson's is a common neuronal disease and usually occurs between the ages of 55 and 65.
What is Parkinson's?

© logo3in1 - stock.adobe.com
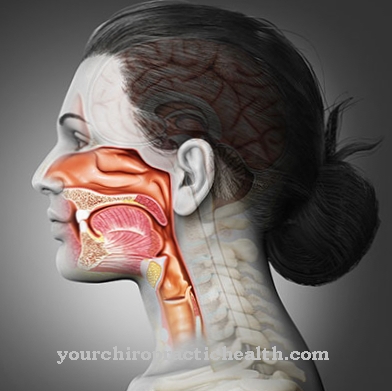
It is a disease of the central nervous system Parkinson's or. Parkinson's disease. Above all, this leads to disruptions in involuntary and voluntary movement sequences. Furthermore, there is a persistent loss of nerve cells in the brain.
The black matter in the brain (so-called basal ganglia) in particular is broken down. They are responsible for the movements and the control of motor skills. In addition, the hormones noradrenaline and adrenaline, as well as the messenger substance dopamine, are formed in them.
As a result, Parkinson's disease leads to a marked lack of exercise or even immobility. Because of the lack of dopamine, the tremor typical of Parkinson's occurs. There is also tension or stiffness in the muscles.
causes
So far the causes are Parkinson's not exactly clarified. These unexplained causes are referred to in medicine as idiopathic Parkinson's syndrome. Only the trigger is known so far. The lack of dopamine (again triggered by the death of the nerve cells) ultimately leads indirectly to the onset of the disease. Medical research has not yet been able to explain why the nerve cells begin to die.
However, there are already known causes of Parkinson's. On the one hand, genetic or hereditary causes play a role. Parkinson's disease often occurs up to the age of 40.Other causes are environmental influences such as poisoning, manganese and carbon monoxide (occurs when smoking).
Other diseases (metabolic disorders, brain tumors, trauma) can also be considered as causes. In addition, some drugs are suspected of causing Parkinson's disease. These include drugs that lower blood pressure and neuroleptics.
Symptoms, ailments and signs
The first symptoms of the disease can appear long before the typical symptoms, without suspecting a connection to Parkinson's. These early onset disorders include, for example, a decrease in the ability to smell, muscle and joint pain, slowing down of routine activities in everyday life, visual disturbances, fatigue, exhaustion or depression.
However, since these symptoms can also be assigned to other diseases, they are difficult to associate with Parkinson's. Only in the further course, when the typical symptoms develop, can you see in retrospect that there were already indications of the disease. The main symptoms come slowly and often only appear on one half of the body at first. The movements slow down and reduce.
In the later stages, this can increase to complete immobility. The facial expressions also seem frozen. The steps shrink; The triple steps of the patient are typical. The muscles become stiff (rigidity). When they are at rest they often begin to tremble (tremor). The entire body becomes unstable over time, and standing upright becomes difficult.
Most of the time, those affected hold themselves slightly bent forward and can only walk by shuffling. It is characterized by the difficulty of starting a movement, so that several attempts are needed to get up or start walking. Bladder weakness, constipation and increased salivation can also be noticeable symptoms.
Diagnosis and course of disease
The course of the disease of Parkinson's happens relatively slowly. However, the course can differ from case to case. It is also decisive whether a therapy or treatment is carried out or not. With good medical treatment, the quality of life and life expectancy in Parkinson's disease can be significantly increased.
The further prognosis of the disease depends on the advanced stage of the disease. A complete cure for Parkinson's is not yet possible. With proper treatment, mental and motor decline can be delayed or slowed for more than twenty years. Still, death from Parkinson's is unfortunately inevitable. Those affected mostly die of pneumonia or other respiratory infections as a result of the disease.
Complications
Parkinson's disease does not always have to be associated with serious complications. With professional therapy, a life without the need for care is definitely possible for a long time. In some cases, however, the affected people suffer from serious consequences.
Three to four Parkinson's disease patients experience swallowing disorders during the illness. These, in turn, can cause malnutrition. There is also the risk that bacteria will penetrate the windpipe if swallowed and cause pneumonia as the disease progresses. This is one of the most common causes of death from Parkinson's disease.
The akinetic crisis is another serious complication. It is used in medicine when the Parkinson's patient suddenly becomes completely immobile. In such cases, immediate hospitalization of the patient is required. As a rule, the akinetic crisis rarely shows up. It primarily affects late-stage patients. The complication is usually caused by other diseases such as pronounced febrile infections or surgical interventions.
Sometimes the interruption of the drug treatment for Parkinson's disease is the reason for the serious consequences. During the akinetic crisis, the patient suffers from severe muscle rigidity (rigor) and can neither speak nor swallow. In addition, because he no longer absorbs fluids, his body quickly threatens to dry out. Other common effects of Parkinson's disease are diffuse back pain, joint and muscle pain, sleep disorders, and depression.
When should you go to the doctor?
If the typical early signs of Parkinson's disease appear and do not go away within one to two weeks, a doctor should be consulted. Symptoms such as unusual tremors, rigidity of the limbs or sudden movement disorders indicate the nerve disease. Persistent sleep disorders or psychological complaints that do not seem to have any underlying cause must also be promptly examined by a doctor. The doctor can make a suspected diagnosis using imaging methods such as CT, MRI and positron emission tomography.
If the attempt at therapy with levodopa is successful, this indicates Parkinson's disease. Then the patient is referred to a specialist who can prescribe the necessary medication. If a Parkinson's patient has a stiff muscle and can no longer swallow his pills, relatives must call an emergency doctor. Medical advice is also required in the case of confusion, delusions or hallucinations. The family doctor or a neurologist is responsible. In addition, physiotherapists, surgeons and, depending on the nature and severity of the symptoms, alternative doctors are also involved in the treatment of the nervous disease.
Treatment and therapy
The therapy of Parkinson's is primarily based on early detection and treatment. Since there is currently no cure for Parkinson's, the goals of treatment are mainly to be found in the area of general improvement in quality of life. The aim is to reduce the mental, emotional and motor complaint symptoms. The aim is to ensure that the person concerned can maintain their own independence for as long as possible.
Therapies based on drugs and physiotherapy (including physiotherapy) are used. But a change in diet can also have a supportive effect. The drugs (levodopa and dopamine agonists) are designed to compensate for the lack of dopamine. Furthermore, deep brain stimulation with high frequency can also be used for therapy. This quite new procedure is supposed to stimulate and stimulate the affected brain regions without destroying nerve cells. However, only the symptoms are treated here and the actual Parkinson's disease is not cured.
In the future, however, there could be therapy methods based on stem cell transplantation (stem cell therapy) so that the dead nerve cells are replaced by new and cultivated cells. A low-fat diet, plenty of drinking and sufficient exercise, such as hiking and swimming, have proven helpful.
Aftercare
The peculiarity of Parkinson's disease means that follow-up care cannot prevent its recurrence. This objective is commonly known in tumors. Parkinson's, on the other hand, cannot be cured. Rather, the symptoms progress slowly.
The purpose of scheduled examinations after a diagnosis is to eliminate complications and enable the patient to lead a symptom-free life. Continuous treatment is therefore necessary, the extent of which depends on the respective complaints. Doctor and patient agree on the rhythm of the examination.
The follow-up includes an intensive discussion about existing complaints. This is followed by a targeted physical examination. If the sick person is at an advanced stage, the typical signs can often be seen at first glance. Some doctors may order neuropsychological exams from time to time.
The EEG and positron emission tomography (PET) are also informative. With the last method, the metabolic activities of the nerve cells can be mapped. In addition, drugs play an important role in therapy. By taking them, patients usually prevent a dopamine deficiency.
Follow-up care includes regular treatments by physiotherapists, speech therapists and psychologists. The doctor prescribes these treatments if there are restrictions in movement, breathing or articulation as well as mental recovery.
You can find your medication here
➔ Medicines to calm down and strengthen nervesOutlook & forecast
Parkinson's now offers a relatively good prognosis. Although the disease is progressive, i.e. with increasing symptoms, it can be treated well with modern medication and therapeutic measures. Forms of therapy such as brain wave stimulation or stem cell therapy could further improve the prognosis in the future. Parkinson's patients are currently dependent on pain relievers and other drugs. They also need support in everyday life and are no longer allowed to perform various activities such as driving a car. All of these things affect the quality of life.
The prospect of a symptom-free life is not given. However, those affected can live with the disease for several decades. The prognosis depends on the stage at which the disease is diagnosed and the constitution of the patient. Young people can overcome strenuous therapies quickly, but they also have to live with the disease for many years and accept more and more losses over the course of their lives.
Basically, it is important to start therapy early. The prognosis is made by the responsible neurologist or another specialist. It must be regularly adjusted to the current state of health of the patient. In addition to the prognosis, the patient is given comprehensive advice and information about current treatment methods.
You can do that yourself
Even small changes in everyday life can help maintain the quality of life with Parkinson's for a long time. A safe living area reduces the risk of falls and injuries: classic tripping hazards are carpets, door sills and loose cables, handrails should be attached to stairs. Grab bars are particularly important in the bathroom next to bathtubs, showers and toilets, and non-slip rubber mats ensure a safe stand.
Shower stools, a raised toilet and, if necessary, a height-adjustable washstand simplify daily personal hygiene. Clothing with Velcro and zip fasteners is more suitable for taking off and putting on independently than clothing that has to be buttoned. If it is difficult to tie your shoes, slippers are a good alternative. A long shoehorn makes it easier to slip on.
The trade has a large number of other aids such as special cutlery, cap openers and drinking aids ready for use in the household. In order to maintain the highest possible mobility and coordination skills, gymnastics exercises should be carried out daily. Special exercises train facial expressions, gestures and fine motor skills of the hands.
A balanced diet provides the body with all the vital substances it needs and helps maintain body weight. Parkinson's patients should take the time to eat and drink, chew the food well, and keep the head and body upright. Thorough oral hygiene prevents tooth damage, bad breath and inflammation caused by food residues.

.jpg)


.jpg)
.jpg)


















.jpg)


