As persistent ductus arteriosus is the term used to describe the postnatal period in which the connection between aorta and pulmonary artery remains open. The earliest possible diagnosis and appropriate therapy prevent complications such as, in the worst case, death of the newborn. If the closure is successful and complete, no further complications are to be expected.
What is a persistent ductus arteriosus?

© SciePro - stock.adobe.com
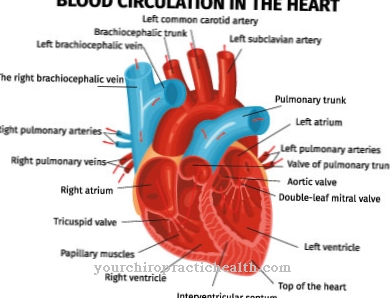
Of the persistent ductus arteriosus refers to a heart defect in the newborn child. Prenatally there is a connection between the aorta and the pulmonary artery, which bypasses the unborn child's pulmonary circulation (right-left shunt). Usually, a postnatal increase in oxygen levels in the blood causes the connection to contract and then recede.
This should be done within the first three days after giving birth. This is not the case in around 30 percent of all infants born before the 31st week of pregnancy. If the duct remains open, a shunt reversal occurs (left-right shunt).A persistent ductus arteriosus is when the connection remains open for more than three months after birth.
The persistent ductus arteriosus makes up five to ten percent of all congenital heart defects and often occurs in combination with other heart defects. Female newborns are two to three times more likely to be affected than males.
causes
The cause of the persistent ductus arteriosus is unclear. However, there is a higher incidence in premature babies, especially those with low birth weights, and also in the case of perinatal oxygen deficiency and births at high altitudes. Asphyxia, i.e. a threatened state of asphyxiation due to a drop in the oxygen content with simultaneous retention of carbon dioxide, can also lead to the ductus remaining open.
Some children do not spontaneously adjust their breathing to the changed circumstances after birth, which is known as respiratory adjustment disorder. Another cause can be chromosomal aberrations such as trisomy 21 or trisomy 18. In the course of rubella embryopathy, in which the rubella virus is transmitted from the mother to the fetus, the ductus can also remain open. A familial occurrence is usually not the case.
Symptoms, ailments & signs
Symptoms depend on the size of the shunt. A small passage usually remains symptom-free. With greater gait, a typical heart murmur can be heard during auscultation, which is most pronounced in the left upper thorax. In addition, exertional dyspnea, tachycardia, breathing difficulties, cyanosis, fatigue, and poor growth, as well as apnea and bradycardia, occur in premature infants.
In extreme cases, recurrent respiratory infections, congestion-related heart failure or, in the elderly, ductus calcifications and aneurysms can occur. Another complication is inflammation of the inner lining of the heart or arteries, which can lead to septic embolisms and lung abscesses.
A symptom-free course has a good prognosis, but carries a lifelong risk of endocarditis. A long walk can result in pulmonary hypertension and irreversible changes in the pulmonary vessels.
Diagnosis & course of disease
There are several diagnostic options. A prenatal diagnosis is not possible because the ductus is open in all unborn babies. If a persistent ductus arteriosus is suspected, various procedures are used. When measuring the pulse, a pulsus celer et altus can be indicative as a sign of a large blood pressure amplitude. The typical, permanent heart murmurs can be clearly heard during auscultation.
Depending on the pressure and volume load, signs of hypertrophy of the heart are visible in the ECG. An enlargement of the left heart can also be seen in the chest x-ray with a large shunt. The echocardiogram and the examination using a cardiac catheter can show the ductus and accompanying anomalies. In the differential diagnosis, arterio-venous fistulas, a ventricular septal defect and peripheral pulmonary stenosis can be excluded.
Complications
The ductus arteriosus is important prenatally in order to connect the pulmonary circulation with the body circulation, because lung breathing is not yet possible. Only after birth does the ductus arteriosus close automatically, creating a separate pulmonary circulation that is separate from the body's circulation. Complications that can occur due to an untreated persistent ductus arteriosus depend on the size of the ductus and the level of development of the newborn.
Smaller connections between the two blood circulation systems can be completely symptom-free and do not require immediate treatment. With larger connections between the two bloodstreams, blood flows from the aorta into the pulmonary artery, increasing pulmonary blood pressure. Typical consequential damage can result in irreversible sclerosis of the pulmonary vessels, which make pulmonary high blood pressure irreversible, it is more or less fixed.
Further consequential damage is an expansion (dilation) of the left atrium and the left ventricle due to the higher degree of filling in the left heart. In the long term, the changes in the heart lead to heart failure. In newborns with a relatively large, persistent ductus arteriosus, it is therefore advisable to separate the two blood circulation systems by means of a small operation. As a rule, such interventions can even be carried out in a cardiac catheterization laboratory, so that surgical treatment is not required.
When should you go to the doctor?
This disease always requires a medical examination and further treatment. In the absence of treatment, the disease usually leads to premature death or other life-threatening complications. A doctor should usually be consulted if the person concerned suffers from relatively loud and clearly audible heart murmurs.
This can also lead to pain in the heart, with this pain being accompanied by severe breathing difficulties or a blue discoloration of the skin. Severe exhaustion or slow development in children can also indicate this disease and should always be examined by a doctor. Furthermore, the disease leads to heart failure, so that the performance of the patient decreases and the patient appears tired or sluggish.
The condition can be diagnosed by a general practitioner. However, further treatment is carried out by a specialist doctor. Whether this will lead to a reduced life expectancy cannot generally be predicted. The earlier treatment is given, the higher the likelihood of a positive course of the disease.
Treatment & Therapy
Early diagnosis and therapy are essential, especially in premature babies and newborns with a low weight, as both comorbidities and mortality are significantly higher in these due to the hemodynamic instability. A persistent ductus arteriosus should always be closed to minimize the risk of endocarditis.
The therapy of the persistent ductus arteriosus takes place in different ways. Prostaglandin synthesis inhibitors can be used to treat drugs. Under no circumstances should these be administered during pregnancy, as the ductus must remain open prenatally. In the case of premature births, drug therapy is usually always used. There are special preparations for this which can be used for births before the 34th week of pregnancy.
A minimally invasive treatment method is the insertion of a coil or an umbrella over a cardiac catheter, which also closes the ductus. In contrast to drug therapy, this method is more likely to be used in older children.
The ductus can be ligated surgically. The mortality rate for this procedure is one percent in childhood and twelve percent in adulthood. Spontaneous closure of the duct is possible. If the closure is successful, the newborn has the same prognosis as the normal population. Another endocarditis prophylaxis is advisable for half a year to check the results of the treatment. No follow-up examinations are then necessary.
Outlook & forecast
The best prognosis is with a persistent ductus arteriosus, when the ductus can be closed. The problem is that this disorder shouldn't even occur in a newborn. Usually this connection closes automatically after the birth. In premature babies, however, this mechanism often fails. In rare cases, minimally invasive duct surgery is necessary.
Having to operate on premature babies or newborns because of a persistent ductus arteriosus carries high risks. This is why pediatric cardiologists try to close the ductus arteriosus botalli, which does not close by itself, with a suitable drug, especially in premature children. This preparation inhibits the production of prostaglandins. Prostaglandin is a messenger substance that affects the immune system. When the prostaglandin level falls, the persistent ductus arteriosus often closes after all.
The administration of “indomethacin” is not possible or successful in every case. If this method fails, or if it proves to be inapplicable, the non-closed connection between the main artery and the pulmonary artery in the affected infant can only be closed surgically. However, this only happens in older children using a cardiac catheter. If the ductus is sealed, the prospects for a long life are quite good.
The prognosis for a persistent ductus arteriosus is much worse if it occurs together with other heart defects.
prevention
Prophylaxis of the persistent ductus arteriosus is not possible during pregnancy, since the open ductus is essential for the development of the newborn. Various studies examined the effectiveness of individual drugs, but no significant difference could be found.
Another study investigated the connection between phototherapy in premature babies, which is also used for jaundice, and the ductus arteriosus remaining open. However, no clear effectiveness could be determined. As efficient prophylaxis is very difficult or impossible, timely diagnosis and intervention are all the more important for the health of the newborn.
Aftercare
Follow-up treatment is particularly necessary after surgical closure of the persistent ductus arteriosus. After the operation, the patient is transferred to the intensive care unit for observation. If a heart catheter has been placed on a leg, it is important not to move it independently at the beginning. Heavy physical exertion should be avoided in the first week after the intervention.
To prevent an infestation with harmful bacteria, appropriate drugs are administered intravenously as a preventive measure. The patient is also given heparin. As part of the follow-up care, the patient must take clopidogrel for three months and acetylsalicylic acid (ASA) for six months.
These drugs are given to counteract the formation of blood clots on the materials used. Administered antibiotic agents protect the heart and blood vessels from inflammation. One day after the procedure, x-rays will be taken to check. A swallow echo examination takes place after about six months.
If any abnormalities become apparent during the follow-up, they must be clarified by a doctor as soon as possible. Regular follow-up examinations should be carried out to ensure the success of the treatment. Only a few years later, if there are no symptoms, can these examinations be completely dispensed with. Whether this is also possible for children who have been treated with a cardiac catheter cannot be clearly stated due to a lack of long-term experience.
You can do that yourself
The persistent ductus arteriosus in newborns can be treated with the exact dosage of medication or with an operation. The parents of the child concerned should follow the doctors' instructions exactly in everyday life. Infections and other illnesses should be avoided whenever possible, especially in the early stages after the birth.
If the ductus arteriosus is diagnosed or if this heart defect is suspected, it is very important to pay attention to the murmurs of the newborn's heart. Such observations, along with fever or other symptoms, indicate the medical problems. Blood pressure also plays a role. Regular follow-up checks are essential for parents. This is the only way to check whether the child is healthy and can grow up normally. The dates for the examinations must be strictly adhered to.
If an operation is performed, further doctor's appointments will also follow. At the same time, parents can watch their child carefully. This enables them to recognize possible problems such as secondary injuries, inflammation or a curved back in good time. In such cases, you should not wait for the next appointment, but consult a doctor as soon as possible. It is also important that the newborn is not exposed to excessive stress.


.jpg)
.jpg)
.jpg)





















