The antibiotic Piperacillin belongs to the group of penicillins. It is used to treat bacterial infections.
What is piperacillin?

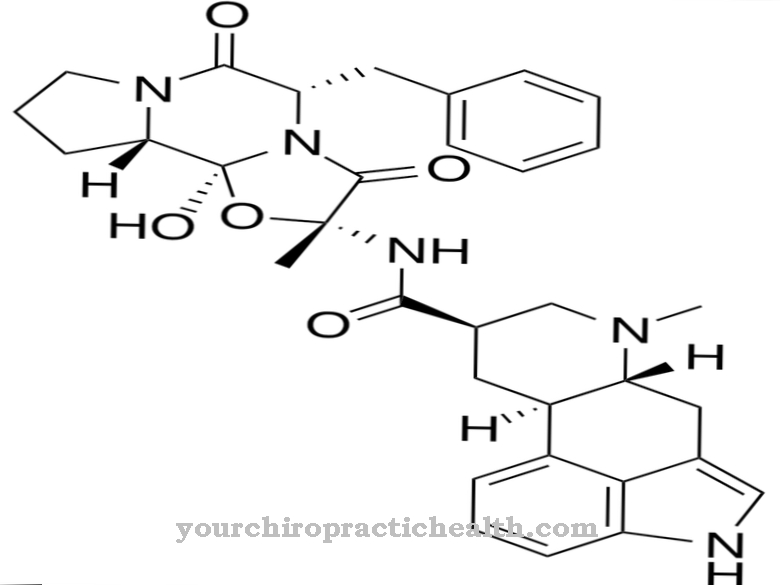
Piperacillin is an antibiotic that belongs to the group of penicillins. More precisely, it is acylaminopenicillin. In addition, piperacillin forms a beta-lactam antibiotic that has a four-membered lactam ring in its structural formula. Of all penicillins, the spectrum of activity with piperacillin is the best.
Penicillins such as piperacillin are the oldest antibiotic agents that are used in medicine. In 1928 the Scottish bacteriologist Alexander Fleming (1881-1955) discovered penicillin by chance. At the time, Fleming was working at St. Mary's Hospital in London with staph bacteria on a bacterial nutrient plate, which he left unattended at times. On his return, the scientist found a mold called Penicillium notatum growing on the agar plate. On the other hand, there was no bacterial growth in the vicinity of the fungus.
The active ingredient had bactericidal properties and was named penicillin by Alexander Fleming. Penicillin developed its positive effect particularly during the Second World War, so that a large number of wound infections could be treated successfully.
Today, however, many bacterial strains are resistant to penicillin. Nevertheless, penicillins such as piperacillin are still used successfully. Piperacillin works against all infections caused by sensitive bacteria.
Pharmacological effect
Piperacillin has the typical mode of action of penicillin. The antibiotic inhibits the build-up of the bacteria cell wall, which leads to their death. The effects of piperacillin surpass the properties of benzylpenicillin. There is a bactericidal (bactericidal) effect against enterobacteria, anaerobes and gram-negative rods. However, there is also a worse effect against gram-positive cocci than with benzylpenicillin. Nevertheless, the bactericidal effect of piperacillin is sufficient and can be compared with the effect of amoxicillin.
Piperacillin can be destroyed by beta-lactamases, which are special bacterial enzymes. For this reason, medicine usually combines piperacillin with other bacteria-killing antibiotics that are able to kill bacteria with enzymes of this type.
Medical application & use
The use of piperacillin is suitable for numerous bacterial infections, which can take both an acute and a chronic course. These include a. Diseases caused by Gram-negative rods such as cystitis (inflammation of the bladder), urethritis (inflammation of the urethra), or pyelonephritis (inflammation of the kidneys). Piperacillin is also effective for infections of the biliary tract, intra-abdominal abscesses, inflammation of the peritoneum (peritonitis), pneumonia in patients with artificial ventilation, gynecological infections such as adnexitis or inflammation of the uterine lining (endometritis).
Further areas of application are nosocomial infections caused by the bacterial species Pseudomonas aeruginosa, inflammation of the inner lining of the heart (endocarditis), severe sepsis (blood poisoning), joint and bone infections such as osteomyelitis (inflammation of the bone marrow) as well as infections of skin and soft tissues after burns, accidents or Operations.
Piperacillin is used exclusively through infusions or injections. Oral ingestion in the form of a tablet is not suitable because the drug is not acid-resistant. Taking pills would destroy the antibiotic. The half-life of piperacillin is 60 minutes. In principle, piperacillin can be used at any age.
Risks & side effects
The administration of piperacillin can cause undesirable side effects in some patients. However, this is not the case for every person as there are great individual differences. The most common side effects include inflammation of the mucous membranes, allergic reactions, rashes, itching, reddening of the skin, headaches and an increase in blood urea concentrations.
In the case of high dosages, bleeding on the mucous membrane is also possible. Sometimes joint pain, drug fever, serum sickness, swelling of the throat, kidney inflammation, allergic vascular inflammation, Stevens-Johnson syndrome and a lack of hemoglobin appear.
In the early stages of piperacillin treatment, in particular, severe diarrhea that lasts for a long time can be seen. This can be the life-threatening bowel disease pseudomembranous colitis.
An outbreak of nettle rash is considered an indication of a penicillin allergy. In this case, treatment with the antibiotic must be stopped immediately. If the patient suffers from hypersensitivity to penicillin or cephalosporin, therapy with piperacillin should be avoided. The administration of penicillin is also not recommended during pregnancy and while breastfeeding, as there is no precise information about the safety of the agent during this period.
In addition, attention must be paid to interactions with other drugs. This is especially true for other penicillins or cephalosporins. If taken at the same time, it delays their breakdown, which leads to a prolonged effect. Piperacillin also increases the level of methotrexate in the blood. The effect of piperacillin can be increased by administering non-steroidal anti-inflammatory drugs such as salicylates, phenylbutazone, sulfinpyrazone or indomethacin. The same applies to the gout drug probenecid.