Of the sudden infant death syndrome was for a long time an unfathomable phenomenon for science, from which thousands of babies died every year. But meanwhile at least risk factors can be identified and precautionary measures can be taken to reduce the risk of this terrible event. However, cot death is still the most common type of death for small children before the age of one in Germany, to which around 300 babies fall prey every year.
What is sudden infant death syndrome?

© thingamajiggs - stock.adobe.com
A sudden infant death syndrome always occurs when an infant dies completely unexpectedly and unexpectedly without previous signs of illness or abnormal behavior and an autopsy cannot provide any clues as to the cause of death.
As a rule, death occurs during the night and is only noticed after some time, since the noisy and motionless baby is viewed by parents as sleeping. Those deaths that occur surprisingly and suddenly but can be explained and proven medically, such as heart failure or a creeping infection, are not designated as sudden infant death syndrome.
causes
Of the sudden infant death syndrome has occupied medicine for decades and still raises more questions than it gives answers. However, there are now a number of - even if not 100% verifiable - theses and assumptions that provide reasons for the sudden death.
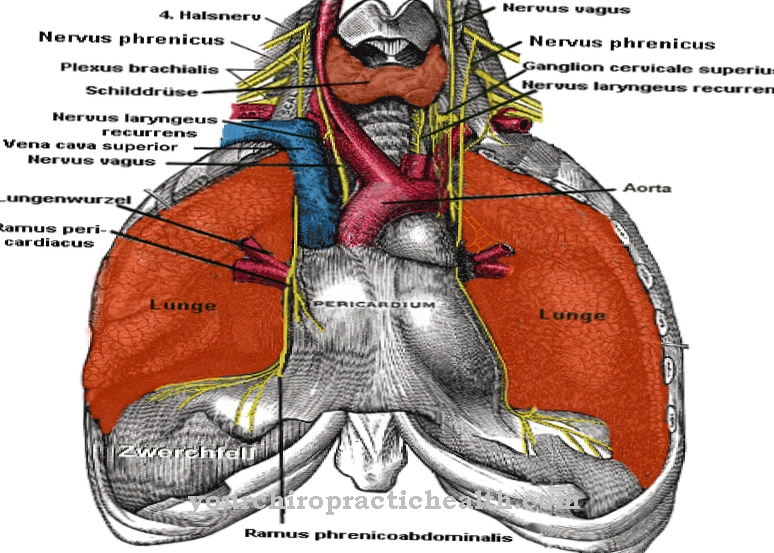
The most recognized of these is that of suffocation of the child through an abrupt cessation of the natural respiratory reflex. Since this mostly happens during sleep, the babies do not wake up and therefore cannot give any warning signs. However, the exact causes for the cessation of breathing are still based on insufficiently substantiated theories.
E.g. sleeping on your stomach has been reported as an increased risk of breathing suspension. Even involuntary, self-inflicted asphyxiation through a pillow or blanket is a possible cause of death for many medical professionals, since most cases occur around the 100th day of life and therefore in a phase in which children are increasingly random and no longer only move purely out of reflex and get caught in the pillow or blanket.
Symptoms, ailments & signs
The fatal aspect of sudden infant death syndrome is that it usually occurs without any clear symptoms or signs in advance. Most of the parents concerned find the children unexpectedly dead in bed. Sudden infant death syndrome is therefore a diagnosis of exclusion if no other clearly identifiable disease that caused the death could be found.
Accordingly, there are no clear signs of impending infant death. Nevertheless, experts can now identify some risk factors that make children appear potentially at risk. However, the individual case must always be discussed with the pediatrician. Many affected children have died in connection with a respiratory infection.
Accordingly, parents should insist on a thorough investigation by a specialist in the event of unclear, persistent or constantly recurring signs of an infection. It has also been found that premature infants and those with a generally low birth weight tend to be more likely to be affected by infant death. The same applies to children whose mothers smoked during pregnancy or after giving birth.
If such risk factors apply, parents should definitely discuss them openly with their doctor. If anything is unclear or if there is an individually increased risk, he or she can prescribe a so-called monitor that monitors vital functions during sleep. Since these are recorded and also give an alarm in the event of changes, the devices can also help to identify possible signs and initiate further examinations.
Diagnosis & course of disease
As a cause of death in the case of sudden infant death syndrome even with an autopsy cannot be determined, a diagnosis can actually only be made unambiguously by excluding all other possible causes of death.
This means that often several experts, such as the pediatrician, a pathologist, and in some cases also the forensic doctor, since a crime cannot always be ruled out, have to examine the deceased child for all sorts of possible causes of death.
Only after all other possibilities have been ruled out and the medical history of the baby has been thoroughly examined is sudden infant death syndrome stated as the official cause of death.
Complications
Sudden infant death syndrome leaves relatives of the deceased child - above all the parents - emotional wounds that can lead to complications. The shock reactions and the resulting depression not infrequently lead to incapacity for work, ill-considered skipping actions or lead to drug addiction or the like, if those affected are left alone with their shock.
Studies have shown that sudden infant death syndrome increases the risk of self-inflicted death in affected parents. The maternal suicide rate quadruples within the first few years after the event. Fathers were found to have an increased risk of accidents and an increased willingness to commit suicide.
In addition, the life expectancy of parents who have suffered sudden infant death syndrome is reduced on average. The risk of various diseases is increased. This includes cancer and cardiovascular diseases, which lead to secondary damage and complications.
The fact that the cause of sudden infant death syndrome often remains unclear puts a lifelong burden on the parents. If the event is not processed - through psychological measures and therapies - the search for the reason or an alleged meaning of the incident manifests itself psychologically. This can lead to a very limited world of experience because all resources are devoted to thoughts about the deceased child. As a result, social structure, job and personal interests are neglected.
prevention
Since, in addition to the baby's prone position at night and getting caught in pillows and blankets, smoking during pregnancy also increases the risk of a sudden infant death syndrome, according to studies, increased many times over, experts strongly advise against it.
In order to avoid the child lying prone, care should be taken to ensure that they fall asleep lying on their back in the evening. However, the prone position should not be completely trained for the child, but on the contrary, with regard to the correct lying on the stomach, should be practiced, otherwise complications can arise from an involuntary rotation on the stomach.
In addition, the use of a special sleeping bag for small children is recommended, which does not require any pillows or blankets lying around. Breastfeeding also has a positive effect on the baby and can also slightly reduce the risk of sudden infant death syndrome.
Thanks to the newly gained knowledge of research and empirical research, many risk factors for sudden infant death syndrome can already be identified and minimized through correct behavior. Nevertheless, the education, especially of young mothers, about such risks and methods of prevention in Germany still leaves much to be desired.
Aftercare
The first point of contact after sudden infant death syndrome is emergency pastoral care. In conversation with a trained supervisor, the relatives receive support and advice on self-help groups and other measures. As part of the follow-up care, the doctor responsible asks whether care is necessary. Many relatives would like to personally say goodbye to the child.
Religious parents often value the child's blessing. Emergency baptism can be carried out by all baptized Christians as long as the child has not died long ago. Siblings of the deceased child must be informed in a child-friendly manner. It is best for parents to contact the local doctor, who will find the right words based on their experience. In the long term, marriage counseling can also be useful for the child's parents.
Often the marriage is exposed to a serious crisis after the death of the child. Coming through the grief is an important aspect of processing. Relatives who feel left alone with their grief turn to a therapist or a support group. If the mother becomes pregnant again after some time, questions about the cause of death of the child should also be clearly clarified in order to relieve the parents of the fears of a new incident.
When should you go to the doctor?
If sudden infant death occurs, no doctor can save the infant. This is because the baby's death is usually not determined immediately, but rather the next time the parents check on him - even a few minutes are enough and no medical help can save the baby. In such cases, a doctor must intervene immediately after the breathing and heartbeat have stopped. Therefore, the only option that remains is to closely monitor babies at increased risk of sudden infant death syndrome. At best, they stay in the hospital until the risk is almost gone.
In this way, they can be connected to medical monitoring equipment that will immediately sound the alarm if the baby shows critical signs. In addition, the paediatricians are always present here and can initiate resuscitation in an emergency.As soon as a baby is allowed to go home at an increased risk, the best prevention is to monitor it here too and to instruct parents on what to do if an emergency occurs. Furthermore, the baby should see the pediatrician regularly until the risky period is over, so that health problems can be recognized and treated in good time. The doctor cannot reverse sudden infant death syndrome that is noticed too late, but he can help to provide prevention. Affected parents should seek psychological or pastoral help.
You can do that yourself
Sudden infant death syndrome often hits families completely unexpectedly. Since the diagnosis of sudden infant death syndrome is a diagnosis of exclusion, it means that no other illnesses that could have caused the death could be found in the child. Accordingly, no measures that could provide absolute security are possible in the area of self-help in everyday life.
Because to this day it has not been conclusively clarified what exactly could have caused the death of the child. Even if there is still no scientific clarity about the exact causes, studies over the years have provided some indications that may prevent cot death. The supine position is still considered to be significantly safer compared to the prone position. As long as parents can influence the child's sleeping position, sleeping the baby lying on its back is probably safer in everyday life. Parents should also avoid covering their child too warmly in bed or even putting blankets, towels or cuddly toys in bed that the child could consciously or unconsciously pull over their head or into the area of their nose.
Studies have shown that children with low birth weights and children of smokers tend to die more often from sudden infant death syndrome. Such known risks should therefore be discussed openly with the pediatrician. If necessary, they will prescribe a special monitor for everyday use at home, which monitors the child's vocal functions during their bedtime.



.jpg)